Overview
Amenorrhea is the absence of menstruation and is commonly defined as missing one or more menstrual periods. It is not a disease itself but a sign of an underlying condition, natural body process, or hormonal change.
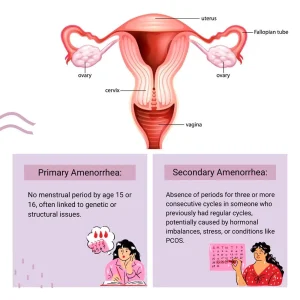
There are two main types of amenorrhea. Primary amenorrhea occurs when a person has not started menstruating by age 15. This form is often related to hormonal imbalances, genetic conditions, or problems with the development of reproductive organs. Secondary amenorrhea refers to the absence of three or more consecutive menstrual periods in someone who previously had regular cycles. Pregnancy is the most common cause of secondary amenorrhea, but hormonal issues and certain medical conditions can also be responsible.
Treatment for amenorrhea depends on identifying and addressing the underlying cause. In many cases, menstrual cycles return once the cause is treated or managed.
Symptoms
The main sign of amenorrhea is the absence of menstrual periods. Depending on the underlying cause, other symptoms may occur alongside missed periods.
These may include:
-
Milky discharge from the nipples
-
Hair loss
-
Headaches
-
Vision changes
-
Excess facial or body hair
-
Pelvic pain
-
Acne
The presence of additional symptoms can help healthcare professionals determine the cause of amenorrhea.
When to see a doctor
Consult a healthcare professional if you have missed three or more menstrual periods in a row or if you have never had a menstrual period by age 15. Early evaluation can help diagnose potential hormonal, structural, or medical conditions and reduce the risk of long-term complications.
Causes
Amenorrhea can occur for many reasons. Some causes are a normal part of life, while others may signal an underlying health issue or side effect of treatment.
Natural causes of amenorrhea include pregnancy, breastfeeding, and menopause. These situations naturally suppress menstrual cycles and do not usually require treatment.
Hormonal birth control methods can also lead to amenorrhea. Some people using oral contraceptives, injections, implants, or certain intrauterine devices may stop having periods. After stopping hormonal contraception, it may take time for normal ovulation and menstruation to return.
Certain medications can interfere with menstrual cycles, including:
-
Antipsychotic medications
-
Chemotherapy drugs
-
Some antidepressants
-
Blood pressure medicines
-
Allergy medications
Lifestyle factors can significantly affect menstruation. Very low body weight can disrupt normal hormone production and stop ovulation. Eating disorders such as anorexia or bulimia are common contributors. Excessive physical activity, especially in sports that require intense training, can also lead to amenorrhea due to low body fat, high energy use, and physical stress. Emotional or mental stress may temporarily affect the brain’s hormone control centers, stopping ovulation and menstruation.
Hormonal imbalances are another major cause. Conditions such as polycystic ovary syndrome can lead to consistently high hormone levels that interfere with normal cycles. Thyroid disorders, whether overactive or underactive, can also affect menstruation. In some cases, a benign tumor of the pituitary gland can disrupt hormone signaling. Premature menopause, when ovarian function declines before age 40, can also cause periods to stop.
Structural problems involving the reproductive organs may prevent menstruation. Uterine scarring, such as in Asherman’s syndrome, can develop after certain procedures and block normal menstrual flow. Some people are born without parts of the reproductive system, such as the uterus or cervix, making menstruation impossible. Vaginal abnormalities, including membranes or blockages, can prevent menstrual blood from exiting the body.
Risk factors
Certain factors increase the likelihood of developing amenorrhea.
These include:
-
A family history of amenorrhea or menstrual disorders
-
Eating disorders such as anorexia or bulimia
-
Intense athletic training or competitive sports
-
A history of gynecologic procedures such as dilation and curettage or cervical treatments
Having one or more of these risk factors does not guarantee amenorrhea but raises the likelihood of menstrual disruption.
Complications
Amenorrhea can lead to several health complications, depending on its cause and duration.
Possible complications include:
-
Infertility or difficulty becoming pregnant due to lack of ovulation
-
Increased risk of miscarriage if hormonal imbalances are present
-
Emotional or psychological stress, particularly in adolescents and young adults
-
Bone loss and osteoporosis due to low estrogen levels
-
Increased risk of cardiovascular disease
-
Chronic pelvic pain when structural abnormalities are involved
Early diagnosis and appropriate treatment can help prevent many of these complications.
Prevention
Amenorrhea cannot always be prevented, especially when caused by genetic or structural factors. However, maintaining overall health can reduce the risk in some cases.
Preventive steps may include:
-
Maintaining a healthy body weight
-
Eating a balanced, nutrient-rich diet
-
Managing stress effectively
-
Avoiding excessive exercise without proper nutrition and recovery
-
Seeking early medical care for menstrual irregularities
Monitoring menstrual health and addressing changes early can support hormonal balance and long-term reproductive health.
Advertisement