Overview
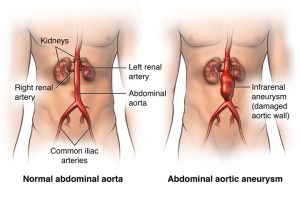
An abdominal aortic aneurysm (AAA) is a localized enlargement or bulging of the abdominal portion of the aorta, the major artery that carries blood from the heart to the rest of the body. The abdominal aorta extends through the chest and into the abdomen, where an aneurysm may form.
A ruptured AAA can lead to severe internal bleeding and is considered a medical emergency with a high risk of fatality.
Diagnosis and Management
Management of an AAA depends on its size and rate of growth, and may range from:
-
Regular monitoring with physical exams and imaging (such as ultrasound or CT scan), to
-
Urgent or emergency surgical intervention in cases of rapid expansion or rupture risk.
Signs and Symptoms
In many cases, abdominal aortic aneurysms develop slowly and without symptoms, making early detection challenging. Some aneurysms remain stable and do not pose an immediate threat, while others may enlarge progressively or rupture.
Symptoms of an expanding or symptomatic AAA may include:
-
A deep, persistent pain in the abdomen or side of the abdomen
-
Back pain
-
A pulsating sensation near the navel (umbilicus)
When to Seek Medical Attention
Seek immediate medical care if you experience:
-
Sudden, severe abdominal or back pain
-
Any symptoms suggestive of a ruptured aneurysm, such as fainting, rapid heartbeat, or low blood pressure
A ruptured abdominal aortic aneurysm requires emergency medical treatment.
Causes
An abdominal aortic aneurysm (AAA) refers to a localized dilation of the abdominal portion of the aorta. Although aneurysms can develop in any segment of the aorta, the abdominal aorta is the most common site.
Potential causes of AAA include:
-
Atherosclerosis: The buildup of lipid plaques and other substances on arterial walls can weaken the vascular structure and contribute to aneurysm formation.
-
Hypertension (High Blood Pressure): Elevated blood pressure increases stress on the aortic wall, promoting degeneration and dilation.
-
Vasculitis and Other Blood Vessel Disorders: Inflammatory conditions affecting blood vessels may damage and weaken the aortic wall.
-
Infection (Mycotic Aneurysm): Although rare, bacterial or fungal infections can invade the aortic wall and cause aneurysmal degeneration.
-
Trauma: Blunt or penetrating abdominal trauma, such as that sustained in motor vehicle collisions, may lead to aneurysm development or expansion.
Risk Factors
Certain factors significantly increase the risk of developing an abdominal aortic aneurysm:
-
Tobacco Use: Smoking is the most significant modifiable risk factor. It damages the vascular endothelium and accelerates atherosclerosis, substantially increasing the risk of AAA formation and rupture.
Clinical note: Men aged 65–75 years with a history of smoking should undergo a one-time screening abdominal ultrasound for AAA.
-
Advancing Age: Risk increases significantly in individuals aged 65 years and older.
-
Sex: Male sex is associated with a higher incidence of AAA compared to females.
-
Ethnicity: Individuals of Caucasian descent have a higher prevalence of AAA.
-
Family History: A positive family history of AAA is associated with increased risk, suggesting a genetic predisposition.
-
Presence of Other Aneurysms: Patients with aneurysms in other vascular regions (e.g., thoracic aorta, popliteal artery) may be at elevated risk for AAA.
Complications
If left untreated, AAAs can lead to serious, potentially fatal complications:
-
Aortic Dissection: A tear between layers of the aortic wall may occur, leading to severe pain and hemodynamic instability.
-
Aneurysm Rupture: Rupture results in life-threatening internal hemorrhage.
Risk correlates strongly with aneurysm size and growth rate.
Signs of Rupture May Include:
-
Sudden, intense, and persistent abdominal or back pain, often described as tearing or ripping
-
Hypotension
-
Tachycardia
-
Signs of shock
-
Thromboembolism: Blood clots may develop within the aneurysm. If embolized, they can obstruct distal vessels, causing ischemia in the lower extremities, kidneys, or abdominal organs.
Prevention
Preventive strategies aim to reduce the risk of aneurysm formation and progression:
-
Tobacco Cessation: Avoid smoking and all forms of tobacco. Secondhand smoke exposure should also be minimized.
Clinician support and pharmacotherapy may be helpful for smoking cessation.
-
Heart-Healthy Diet: Emphasize consumption of:
-
Fruits and vegetables
-
Whole grains
-
Lean proteins (e.g., poultry, fish)
-
Low-fat dairy
Limit intake of saturated fats, trans fats, and sodium.
-
-
Blood Pressure and Lipid Control: Adhere to prescribed antihypertensive and lipid-lowering medications as directed. Regular monitoring is essential.
-
Physical Activity: Engage in at least 150 minutes per week of moderate-intensity aerobic exercise (e.g., brisk walking). Initiate activity gradually, especially in previously sedentary individuals, under clinical guidance.
Advertisement