Overview
Gestational diabetes is a type of diabetes that develops during pregnancy in women who did not previously have diabetes. It occurs when hormonal changes during pregnancy affect how the body uses insulin, leading to elevated blood sugar levels. Gestational diabetes usually develops in the second or third trimester and often resolves after childbirth, but it requires careful management to protect the health of both the mother and the baby.
Symptoms
Gestational diabetes often causes no noticeable symptoms and is commonly detected through routine prenatal screening. When symptoms do occur, they may include:
-
Increased thirst
-
Frequent urination
-
Fatigue
-
Blurred vision
-
Recurrent infections such as urinary tract infections
Because symptoms can be mild or resemble normal pregnancy changes, screening is essential.
Causes
Gestational diabetes occurs when pregnancy-related hormones interfere with the action of insulin. As pregnancy progresses, the body needs more insulin to keep blood sugar levels normal. If the pancreas cannot produce enough insulin to meet this increased demand, blood sugar levels rise, leading to gestational diabetes.
Risk Factors
Several factors increase the risk of developing gestational diabetes, including:
-
Being overweight or obese before pregnancy
-
Family history of diabetes
-
Previous history of gestational diabetes
-
Previous delivery of a baby with high birth weight
-
Maternal age over 25
-
Polycystic ovary syndrome
-
Sedentary lifestyle
Women from certain ethnic backgrounds may also have a higher risk.
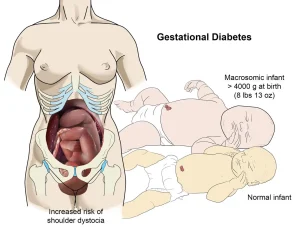
Complications
If not well controlled, gestational diabetes can lead to complications for both the mother and the baby. Possible complications include:
-
High birth weight, increasing the risk of delivery complications
-
Preterm birth
-
Low blood sugar in the newborn after birth
-
Increased risk of cesarean delivery
-
Higher likelihood of developing type 2 diabetes later in life for both mother and child
Proper management significantly reduces these risks.
Prevention
Gestational diabetes cannot always be prevented, but certain steps may help lower the risk:
-
Maintaining a healthy weight before pregnancy
-
Eating a balanced, nutritious diet
-
Engaging in regular physical activity before and during pregnancy
-
Attending all prenatal appointments and screenings
-
Managing blood sugar levels closely if risk factors are present
Early screening, healthy lifestyle habits, and appropriate medical care help ensure a healthy pregnancy and reduce complications associated with gestational diabetes.
Advertisement