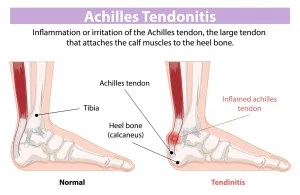
Overview
Diagnosis of Achilles Tendinitis
Diagnosis of Achilles tendinitis begins with a detailed physical examination and may be supported by imaging studies to evaluate the extent of tendon injury and exclude other conditions.
-
Physical Examination:
The healthcare provider gently palpates the Achilles tendon and surrounding structures to assess for tenderness, swelling, thickening, or nodules. Gait, range of motion, and tendon movement during rest and activity are observed to identify functional impairment.
Imaging Studies
-
X-rays:
Although X-rays do not visualize soft tissue directly, they may reveal calcifications within the tendon or bony spurs at the calcaneus, suggesting chronic tendinopathy. X-rays also help rule out fractures or other bone-related conditions. -
Ultrasound:
Ultrasound provides a real-time, dynamic assessment of the tendon’s structure and movement. It can detect tendon thickening, tears, and areas of neovascularization using color Doppler imaging. -
Magnetic Resonance Imaging (MRI):
MRI offers high-resolution images of the Achilles tendon and surrounding tissues, useful for evaluating the severity of degeneration, partial tears, or associated pathologies. MRI is particularly valuable when surgery is being considered.
Treatment of Achilles Tendinitis
Most cases of Achilles tendinitis respond well to conservative management, including self-care and physical therapy. In more persistent or severe cases, advanced procedures or surgery may be required.
Medications
-
Nonsteroidal Anti-inflammatory Drugs (NSAIDs):
Over-the-counter medications such as ibuprofen or naproxen can reduce pain and inflammation. If these are not sufficient, prescription-strength anti-inflammatory medications may be prescribed. -
Topical Nitroglycerin:
A nitroglycerin patch applied directly to the affected tendon may promote healing and provide pain relief. This therapy is typically used daily for 2–3 months.
Physical Therapy
Physical therapy is a cornerstone of treatment for Achilles tendinitis and aims to promote healing, strengthen the tendon, and restore mobility.
-
Exercise Therapy:
Progressive resistance exercises, such as eccentric heel raises or heavy-load training, are effective in treating chronic Achilles tendinopathy. -
Orthotic Devices:
Heel lifts, wedges, or shoe inserts can reduce mechanical stress on the tendon. Heel pads may be used to provide additional cushioning and relieve discomfort.
Advanced and Regenerative Therapies
These newer, minimally invasive treatments may be considered when symptoms persist despite conservative management:
-
Extracorporeal Shock Wave Therapy (ESWT):
ESWT delivers focused shock waves to the tendon to stimulate healing and relieve pain. This noninvasive procedure typically involves several 30-minute sessions and may cause mild bruising, swelling, or discomfort. -
Platelet-Rich Plasma (PRP) Injections:
PRP uses the patient’s own platelets, concentrated and injected into the affected tendon. Growth factors in PRP may accelerate tissue repair. -
Ultrasound-Guided Tenotomy:
A minimally invasive procedure where damaged tissue within the tendon is broken down and removed using a specialized device guided by ultrasound. Post-procedure, patients typically use crutches and a walking boot for several weeks. -
Ultrasound-Guided Tendon Scraping:
This procedure targets abnormal nerves and blood vessels that may contribute to pain. A small incision is made, and the device scrapes the surface of the tendon to denervate and decompress the area, often resulting in rapid pain relief and functional recovery within a week.
Surgical Treatment
Surgery may be recommended if symptoms persist after several months of conservative treatment or in cases of partial or complete tendon rupture. Surgical techniques involve removing degenerated tissue and repairing or reconstructing the tendon. Postoperative rehabilitation is essential for optimal recovery.
Advertisement