Overview
Diagnosis
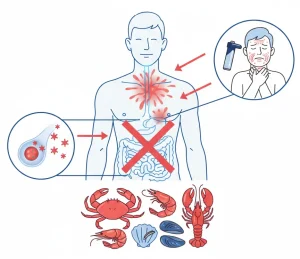
To determine if you have a shellfish allergy, your healthcare provider will review your symptoms and perform a physical exam to rule out other medical issues. A history of allergic reactions shortly after eating shellfish may indicate an allergy, but symptoms could also result from other causes, such as food poisoning.
Allergy testing is the most reliable way to confirm a shellfish allergy. Tests may include:
-
Skin prick test: Small amounts of shellfish proteins are pricked into the skin on your arm or upper back. A raised bump or hive at the test site within 15–20 minutes indicates an allergic reaction. Allergy specialists are best equipped to perform these tests.
-
Blood test: Measures the immune system’s response to shellfish proteins by detecting the level of immunoglobulin E (IgE) antibodies in your blood.
If results are unclear, medically supervised food challenges may be conducted under close observation.
Treatment
Avoiding shellfish is the only guaranteed way to prevent an allergic reaction. For people at risk of severe reactions (anaphylaxis):
-
Epinephrine injection: Emergency use of epinephrine (adrenaline) is required if a severe reaction occurs. Prescriptions for auto-injectors like Auvi-Q or EpiPen may be provided, along with instructions for proper use.
-
Carry epinephrine: Keep an injectable epinephrine device with you at all times. Administer at the first sign of a reaction; a second dose may be needed if symptoms return.
-
Seek emergency care: Even after using epinephrine, go to the hospital to ensure symptoms do not recur.
Regularly check the expiration date of your epinephrine auto-injector to ensure it is current and effective.
Advertisement