Overview
Diagnosis of Anal Fistula
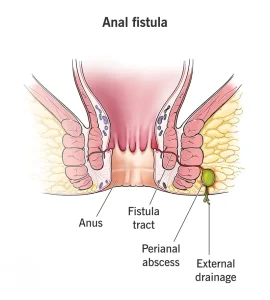
Anal fistulas are abnormal connections between the anal canal and the skin around the anus. Diagnosis usually involves:
-
Medical history and physical exam: Your doctor will assess symptoms such as pain, swelling, discharge, or recurrent abscesses.
-
Probing and visualization: Gentle probing of the fistula tract may be done to determine the path.
-
Imaging tests: MRI or endorectal ultrasound may be used for complex fistulas to map the fistula and plan surgery.
Treatment of Anal Fistula
Treatment focuses on eliminating the fistula and preventing recurrence:
-
Surgical intervention: Most anal fistulas require surgery, such as fistulotomy or seton placement.
-
Antibiotics: May be used temporarily for infection, but are not a definitive treatment.
-
Supportive care: Sitz baths, pain management, and good hygiene help relieve symptoms during recovery.
Key Takeaways
-
Anal fistulas usually require surgical management for long-term healing.
-
Imaging helps assess complexity and guide treatment.
-
Postoperative care is important to prevent recurrence and infection.
Advertisement