Overview
Diagnosis
Diagnosing iron deficiency anemia usually begins with blood tests that check for:
-
Red blood cell size and color, which may appear smaller and paler than usual
-
Hematocrit levels, which show the percentage of blood made up of red blood cells
-
Hemoglobin levels, which indicate how well the blood carries oxygen
-
Ferritin levels, which help measure how much iron is stored in the body
Other diagnostic tests
When blood tests show iron deficiency anemia, additional evaluations may be needed to find the underlying cause. These may include:
-
Endoscopy to look for sources of bleeding in the upper digestive tract
-
Colonoscopy to check for bleeding in the colon or rectum
-
Pelvic ultrasound for people who have periods to look for causes of heavy menstrual bleeding, such as fibroids
Sometimes these tests are done after trying iron supplements to see whether the supplements help improve blood levels.
Treatment
Treatment for iron deficiency anemia focuses on restoring iron levels and addressing the cause of the deficiency.
Iron supplements
Iron tablets are the most common treatment. Liquid iron may be recommended for infants and children. To help improve absorption, you may be advised to:
-
Take iron on an empty stomach if tolerated
-
Avoid taking iron with antacids
-
Take iron with vitamin C
-
Avoid coffee or tea within an hour of taking iron
Iron supplements may cause constipation or dark stools. A stool softener may help. In severe cases, iron may be given through a vein. Rarely, a blood transfusion is needed to quickly restore levels.
It may take several months of daily supplements to rebuild iron stores. Most people begin to feel better within a week of starting treatment.
Treating causes of iron deficiency
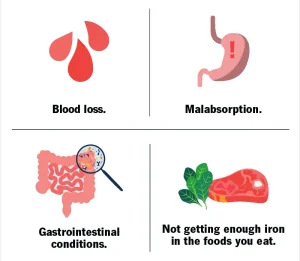
If iron levels do not improve with supplements, the anemia may be due to bleeding or problems absorbing iron. Your healthcare professional will work to find and treat the underlying cause.
Advertisement