Overview
Diagnosis
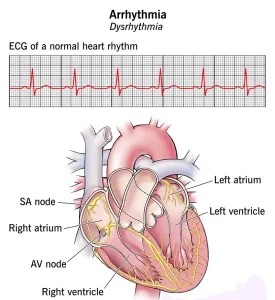
Diagnosing a heart arrhythmia involves a detailed evaluation by a healthcare professional, including a review of symptoms, medical history, and specialized heart tests. The goal is to determine whether the heart’s rhythm is irregular and to identify any underlying conditions contributing to it.
Common diagnostic tests include:
-
Electrocardiogram (ECG or EKG): A quick and painless test that measures the electrical activity of the heart using sensors placed on the chest, arms, or legs. It helps detect abnormal rhythms and heart rate patterns.
-
Holter monitor: A portable ECG device worn for one or more days to continuously record heart activity during normal daily routines.
-
Event recorder: Similar to a Holter monitor, but worn for up to 30 days. You press a button to record when symptoms occur.
-
Echocardiogram: Uses ultrasound waves to create images of the heart’s structure and motion, helping evaluate valve function, heart muscle strength, and blood flow.
-
Implantable loop recorder: A small device placed under the skin in the chest that continuously tracks heart rhythm for long periods, ideal for detecting infrequent arrhythmias.
If no arrhythmia is detected in initial tests, additional procedures may be used to trigger or monitor irregular heart rhythms:
-
Stress test: Monitors heart function during exercise or with medication that simulates physical activity to detect exercise-induced arrhythmias.
-
Tilt table test: Used for fainting spells, this test records heart rate and blood pressure as the body position changes from lying down to standing.
-
Electrophysiological (EP) testing and mapping: Conducted in a hospital setting, this test identifies the source of irregular electrical activity in the heart using catheters with sensors inserted through blood vessels.
Treatment
Treatment for heart arrhythmia depends on the type, cause, and severity of the irregular heartbeat. Some arrhythmias require no intervention, while others need medication, therapy, or surgery to prevent complications such as stroke or cardiac arrest.
Medicines
Medication is often prescribed to manage heart rhythm or rate.
-
People with tachycardia may take drugs to slow the heart rate.
-
Those with atrial fibrillation are often prescribed blood thinners to reduce the risk of blood clots.
Therapies
Non-surgical therapies can help control heart rhythm:
-
Vagal maneuvers: Simple actions such as coughing, holding your breath, or applying an ice pack to the face can slow a fast heartbeat by stimulating the vagus nerve.
-
Cardioversion: Involves delivering controlled electrical shocks to the heart through paddles or patches on the chest to restore a normal rhythm. It is often used when medications and vagal maneuvers fail.
Surgery and Procedures
Advanced cases of arrhythmia may require procedures or implanted devices:
-
Catheter ablation: A minimally invasive procedure using heat or cold energy to create small scars in the heart tissue to block abnormal electrical signals.
-
Pacemaker: A small device implanted in the chest to regulate a slow heartbeat.
-
Implantable cardioverter-defibrillator (ICD): A device placed under the skin that monitors heart rhythm and delivers shocks when life-threatening arrhythmias occur, such as ventricular tachycardia or fibrillation.
-
Maze procedure: Surgical creation of a scar tissue pattern in the upper heart chambers to block erratic electrical signals. It is usually done when other treatments are ineffective or during open-heart surgery.
-
Coronary bypass graft surgery: Performed if coronary artery disease is contributing to the arrhythmia. The surgery reroutes blood flow around blocked arteries to improve circulation.
After treatment, ongoing follow-up is essential. Regular checkups, adherence to prescribed medication, and timely communication with your healthcare team can help manage symptoms and prevent future complications.
Advertisement