Overview
Diagnosis
Diagnosing occupational asthma is similar to diagnosing other types of asthma, but the key difference is determining whether a workplace substance is triggering your symptoms. Your healthcare professional will assess your symptoms, medical history, and workplace exposure to identify the cause.
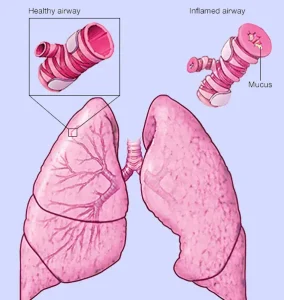
A lung function test is essential to confirm an asthma diagnosis. This test measures how well your lungs work and how easily you can exhale air. Additional tests, such as allergy skin prick tests, blood tests, or X-rays, may be needed to rule out other causes of your symptoms.
Testing your lung function includes:
-
Spirometry: This test takes about 10 to 15 minutes. You’ll take deep breaths and then exhale forcefully into a spirometer, a device that measures how much air your lungs can hold and how quickly you can exhale. Afterward, you may repeat the test following the use of an asthma medication that opens the airways. Improved lung function confirms the diagnosis of asthma.
-
Peak flow measurement: You may be asked to use a small, hand-held device called a peak flow meter, which measures how quickly you can exhale. Slower exhalation suggests airway obstruction. You’ll likely measure your peak flow at different times — during work and outside of work. If your breathing improves when you’re away from work, it indicates occupational asthma.
Tests for causes of occupational asthma:
-
Allergy skin tests: Small amounts of common allergens such as dust mites, mold, plants, latex, and animal dander are scratched into the skin. Swelling or redness shows an allergic reaction. These tests identify biological allergens but cannot measure reactions to chemicals.
-
Challenge test: You inhale a mist containing a small amount of a suspected chemical. Lung function is tested before and after exposure to determine whether it triggers breathing problems.
-
Chest X-ray: Since occupational asthma is a type of occupational lung disease, a chest X-ray may help identify or rule out other job-related respiratory issues.
Treatment
The main goal of treatment for occupational asthma is to prevent symptoms and stop asthma attacks from occurring. Avoiding exposure to the workplace substance causing your symptoms is critical, as even tiny amounts may trigger a reaction once sensitivity develops.
Medications used for occupational asthma are the same as those for other forms of asthma. The right treatment depends on factors such as your age, symptom severity, triggers, and individual response to medication.
Long-term control medicines:
-
Inhaled corticosteroids: These medications reduce airway inflammation and have a low risk of side effects.
-
Leukotriene modifiers: Used as alternatives or additions to corticosteroids, they help control inflammation.
-
Long-acting beta agonists (LABAs): These open the airways and reduce inflammation but should only be used with inhaled corticosteroids for asthma.
-
Combination inhalers: These contain both a LABA and a corticosteroid for effective long-term control.
Quick-relief, short-term medications:
-
Short-acting beta agonists: Used for fast relief during asthma attacks to open airways quickly.
-
Oral and intravenous corticosteroids: Used for severe asthma to reduce inflammation. However, long-term use can cause serious side effects.
If you find yourself using quick-relief inhalers more frequently than prescribed, it may indicate the need to adjust your long-term control medication.
For individuals whose asthma is worsened by allergies, additional allergy treatments may be helpful. These can include:
-
Antihistamines: To block immune system reactions that cause allergy symptoms.
-
Decongestants: To relieve nasal congestion and improve breathing comfort.
Managing occupational asthma effectively requires close collaboration with your healthcare provider, workplace modifications, and consistent use of prescribed medication to maintain healthy lung function.
Advertisement