Overview
Diagnosis
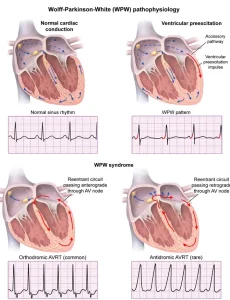
Diagnosing Wolff-Parkinson-White (WPW) syndrome involves identifying the presence of an extra electrical pathway in the heart that causes rapid heartbeats. A healthcare professional evaluates symptoms, performs a physical exam, and uses diagnostic tests to confirm the condition.
Common diagnostic methods include:
-
Electrocardiogram (ECG): The primary test used to detect WPW. It records the heart’s electrical activity and shows characteristic patterns such as a short PR interval and delta waves.
-
Holter monitor: A portable ECG device worn for 24–48 hours to track irregular heart rhythms that occur intermittently.
-
Event monitor: Similar to a Holter monitor but used for longer periods. The device records heart activity when symptoms arise.
-
Electrophysiological (EP) study: A specialized test where thin, flexible wires are inserted into the heart through blood vessels to map its electrical pathways. This helps pinpoint the location of the abnormal pathway and assess the risk of dangerous arrhythmias.
-
Echocardiogram: Uses sound waves to create images of the heart and check for structural abnormalities.
Diagnosis often occurs after an episode of rapid heartbeat, but some people are diagnosed incidentally during a routine ECG.
Treatment
The goal of treatment for WPW syndrome is to prevent episodes of rapid heart rate (tachycardia) and manage symptoms effectively. The best approach depends on symptom severity, frequency, and overall health.
Treatment options include:
-
Vagal maneuvers: Simple actions such as coughing, bearing down (Valsalva maneuver), or immersing the face in cold water can sometimes stop an episode by stimulating the vagus nerve to slow the heart rate.
-
Medicines: Antiarrhythmic drugs such as procainamide or amiodarone may be used to control heart rhythm. However, medication is often considered temporary or for those who cannot undergo procedures.
-
Catheter ablation: The most common and effective treatment. During this minimally invasive procedure, a catheter delivers radiofrequency energy to destroy the extra electrical pathway. This often cures WPW permanently.
-
Cardioversion: For severe or unstable cases, an electric shock may be used to restore normal heart rhythm.
-
Lifestyle modifications: Avoiding stimulants like caffeine and certain medications that can trigger arrhythmias may help reduce episodes.
With successful treatment, most people with WPW syndrome can live normal, active lives without long-term complications. Regular follow-ups with a cardiologist help ensure ongoing heart health and prevent recurrence.
Advertisement