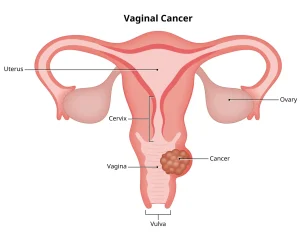
Overview
Diagnosis
Diagnosis of vaginal cancer involves a series of exams and tests to identify cancer cells and determine the stage of the disease.
Pelvic exam
A pelvic exam allows a healthcare professional to inspect the reproductive organs. It may be performed during a routine checkup or if symptoms of vaginal cancer are present. During the exam, the healthcare provider:
-
Examines the outer genital area.
-
Inserts two fingers into the vagina while pressing on the abdomen to feel the uterus and ovaries.
-
Uses a device called a speculum to open the vaginal canal and inspect the cervix and vaginal walls for abnormalities.
Colposcopy
This test involves using a lighted magnifying instrument to closely examine the vagina. Colposcopy helps detect any abnormal changes that may indicate cancer or precancerous conditions.
Biopsy
A biopsy involves removing a small sample of vaginal tissue for testing. The sample is examined under a microscope to confirm the presence of cancer cells. A biopsy is often done during a pelvic or colposcopy exam.
Staging
If vaginal cancer is diagnosed, staging tests are performed to determine the size and spread of the cancer. Staging helps doctors plan treatment and predict recovery outcomes.
Tests for staging may include:
-
Imaging tests such as X-rays, CT scans, MRI, or PET scans to detect cancer spread.
-
Cystoscopy to look inside the bladder.
-
Proctoscopy to examine the rectum.
Vaginal cancer is staged from 1 to 4. Stage 1 means the cancer is limited to the vagina, while stage 4 indicates the cancer has spread to nearby organs or distant parts of the body.
Treatment
Treatment for vaginal cancer depends on the cancer type, stage, and overall health. Most cases are treated with a combination of radiation therapy and chemotherapy, while small localized cancers may be treated with surgery alone.
Radiation therapy
Radiation therapy uses high-energy beams to destroy cancer cells.
-
External radiation: Beams are directed from a large machine outside the body to the cancer site.
-
Internal radiation (brachytherapy): Radioactive materials such as seeds or wires are placed inside or near the vagina for a set period and then removed.
Radiation therapy is often combined with low-dose chemotherapy to enhance its effectiveness. It can also be used after surgery to eliminate remaining cancer cells.
Surgery
Surgery may be recommended for small or localized vaginal cancers. Common surgical options include:
-
Vaginectomy: Removal of part or all of the vagina. This procedure is typically used for small cancers that haven’t spread beyond the vagina.
-
Pelvic exenteration: Removal of several pelvic organs, such as the bladder, uterus, ovaries, vagina, and rectum, when cancer returns or doesn’t respond to other treatments.
If the vagina is completely removed, reconstructive surgery can be performed using skin or muscle from other body parts to create a new vagina. This allows for vaginal intercourse, though the new vagina may have reduced sensation and lubrication.
Other treatment options
When other treatments are not successful, additional options may include:
-
Chemotherapy: Uses powerful drugs to destroy cancer cells, especially when the cancer has spread or returned.
-
Immunotherapy: Helps the immune system recognize and destroy cancer cells, often used for advanced vaginal melanoma.
-
Clinical trials: Offer access to new or experimental treatments that may improve outcomes.
Palliative care
Palliative care focuses on improving quality of life for individuals with cancer. It helps manage pain, side effects, and emotional stress during treatment. A multidisciplinary team of doctors, nurses, and therapists provides this supportive care alongside curative treatments.
Combining palliative care with other treatments can help patients feel better, improve comfort, and often extend survival.
Advertisement