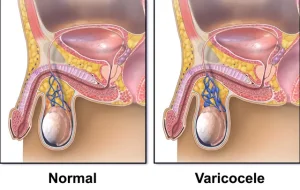
Overview
Diagnosis
Your healthcare provider can diagnose a varicocele through a physical examination of the scrotum by both visual inspection and touch. You’ll likely be examined while lying down and standing up.
When standing, your provider may ask you to take a deep breath, hold it, and bear down, similar to the pressure during a bowel movement. This is called the Valsalva maneuver, which helps make a varicocele easier to detect.
Imaging test
Your healthcare provider may recommend an ultrasound exam to confirm the diagnosis. Ultrasound uses high-frequency sound waves to create detailed images of internal structures. These images can help to:
-
Confirm the diagnosis or better characterize the varicocele
-
Rule out other possible causes of symptoms
-
Detect any lesion or obstruction affecting blood flow
Treatment
In many cases, a varicocele does not require treatment. However, for men experiencing infertility, surgery to correct the varicocele may be part of a fertility treatment plan.
For teenagers or young adults not seeking fertility treatment, annual checkups are often recommended to monitor changes. Surgery may be advised if there is:
-
A testicle that shows delayed growth
-
Low sperm count or other sperm abnormalities (typically assessed in adults)
-
Chronic pain not managed with medication
Surgery
The goal of surgery is to seal off the affected vein, redirecting blood flow to healthy veins. The scrotum has multiple vein systems, so normal blood circulation is maintained.
Possible outcomes after surgery include:
-
The affected testicle may return to normal size or catch up in development
-
Improvement in sperm count and sperm quality
-
Enhanced fertility or improved semen quality for in vitro fertilization
Risks of surgery
Varicocele repair is generally safe but may carry risks such as:
-
Fluid buildup around the testicle (hydrocele)
-
Recurrence of varicocele
-
Infection
-
Artery damage
-
Chronic testicular pain
-
Blood collection around the testicle (hematoma)
When surgery is done mainly for pain relief, results can vary. Some patients may experience worsening or changing pain after surgery, especially if the pain was not directly caused by the varicocele.
Surgical procedures
Two main surgical approaches are used, both requiring general anesthesia and performed as outpatient procedures:
-
Microscopic varicocelectomy: A small incision is made in the groin area. Using a microscope, the surgeon locates and ties off several small veins. The procedure usually lasts 2 to 3 hours.
-
Laparoscopic varicocelectomy: Performed using a small camera and surgical instruments through tiny incisions in the lower abdomen. Because fewer veins need to be tied, the procedure typically lasts 30 to 40 minutes.
Recovery
Pain after surgery is usually mild and may last a few days to weeks. Your doctor may prescribe pain medication initially, then recommend over-the-counter options such as acetaminophen or ibuprofen.
You can typically return to work within a week and resume exercise after about two weeks. Always confirm with your surgeon when it’s safe to resume normal activities or sexual activity.
Alternative to surgery: Embolization
Embolization is a minimally invasive alternative to surgery. A radiologist inserts a small tube into a vein in your groin or neck using local anesthesia and mild sedation.
Guided by imaging, the radiologist places coils or a scarring solution to block the affected veins, redirecting blood flow. The procedure takes about an hour.
Recovery is generally quick, with mild discomfort. Most people return to work within 1 to 2 days and can resume exercise after about a week. Always follow your radiologist’s advice regarding when to resume full activity.
Advertisement