Overview
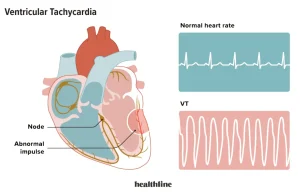
Ventricular tachycardia is a serious heart rhythm disorder in which the lower chambers of the heart, called the ventricles, beat very fast due to abnormal electrical signals. This rapid rhythm prevents the heart from pumping blood effectively, which can reduce blood flow to the brain and other vital organs.
Ventricular tachycardia may last only a few seconds or persist for longer periods. Sustained episodes are medical emergencies and can lead to ventricular fibrillation or sudden cardiac arrest if not treated promptly.
Symptoms
Symptoms of ventricular tachycardia depend on how fast the heart is beating and how long the abnormal rhythm lasts. Common symptoms include:
-
Palpitations or rapid heartbeat
-
Dizziness or lightheadedness
-
Shortness of breath
-
Chest pain or discomfort
-
Fainting or near-fainting episodes
-
Fatigue
-
Sudden collapse in severe cases
Some brief episodes may cause few or no symptoms but still require medical evaluation.
Causes
Ventricular tachycardia is usually caused by damage or abnormalities in the heart’s electrical system. It often occurs in people with underlying heart disease.
Common causes include:
-
Previous heart attack with scar tissue formation
-
Coronary artery disease
-
Cardiomyopathy
-
Heart failure
-
Congenital heart defects
-
Inflammation of the heart muscle
-
Electrolyte imbalances
-
Drug toxicity or side effects of certain medications
In rare cases, ventricular tachycardia can occur in people with structurally normal hearts.
Risk Factors
Several factors increase the risk of developing ventricular tachycardia:
-
History of heart attack
-
Coronary artery disease
-
Heart failure
-
Cardiomyopathy
-
Previous episodes of ventricular arrhythmias
-
Family history of sudden cardiac death
-
Severe electrolyte disturbances
-
Use of stimulant drugs
The presence of multiple risk factors increases the likelihood of serious complications.
Complications
Ventricular tachycardia can lead to life-threatening complications, especially if episodes are sustained:
-
Sudden cardiac arrest
-
Ventricular fibrillation
-
Heart failure
-
Stroke due to poor blood circulation
-
Brain damage from reduced oxygen supply
-
Increased risk of death without timely treatment
Early diagnosis and appropriate management are critical to reducing these risks.
Prevention
Ventricular tachycardia cannot always be prevented, but the risk can be reduced by managing underlying heart conditions:
-
Controlling blood pressure, cholesterol, and diabetes
-
Treating coronary artery disease and heart failure
-
Avoiding smoking and illicit drug use
-
Taking prescribed heart medications as directed
-
Regular follow-up with a cardiologist
-
Implantable cardioverter-defibrillator placement in high-risk individuals
Prompt treatment of heart disease and adherence to medical care plans play a key role in preventing ventricular tachycardia and its complications.
Advertisement