Overview
Diagnosis
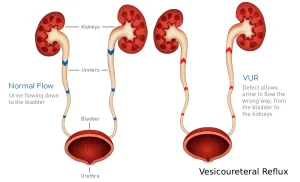
Diagnosis for vesicoureteral reflux involves several steps to confirm whether a child has the condition. The process often begins with a urine test to check for a urinary tract infection (UTI). Additional imaging and diagnostic tests may be needed to evaluate the urinary system in more detail.
Tests used for diagnosis include:
-
Kidney and bladder ultrasound – This imaging test uses sound waves to create images of the kidneys and bladder. It helps identify irregularities and detect swollen kidneys, which may indicate primary vesicoureteral reflux.
-
Voiding cystourethrogram (VCUG) – A specialized X-ray test that shows how urine flows through the bladder and urethra. During the test, a thin tube called a catheter is inserted into the bladder, and contrast dye is injected. X-rays are taken while the bladder fills and empties. This test shows whether urine is flowing backward into the ureters or kidneys.
-
Nuclear scan – This test uses a tracer called a radioisotope to monitor how well the urinary tract is functioning. It involves less radiation exposure than a VCUG but still requires catheter placement.
It is important to choose a medical center experienced in performing these tests, especially for young children, to minimize discomfort and reduce radiation exposure.
Grading the Condition
After testing, healthcare professionals classify vesicoureteral reflux into grades based on severity:
-
Grade 1: Urine backs up only into the ureter.
-
Grade 2: Urine backs up into the ureter and reaches the kidney without causing swelling.
-
Grade 3: The ureter and kidney show mild swelling.
-
Grade 4: Moderate swelling and twisting of the ureter.
-
Grade 5: Severe reflux with significant kidney swelling and twisting of the ureter.
Treatment
Treatment for vesicoureteral reflux depends on the condition’s severity, age of the child, and whether symptoms like UTIs are recurring. Some children with mild reflux outgrow it as they develop.
Medications
Antibiotics are prescribed to treat and prevent urinary tract infections. In mild cases, low-dose antibiotics may be given over time to prevent infection while monitoring the reflux.
Children undergoing medical management require:
-
Regular physical exams
-
Routine urine tests to detect breakthrough infections
-
Occasional bladder and kidney scans to check for improvements
Surgery
Surgery is considered when vesicoureteral reflux does not improve with medication or when UTIs with fever persist. The surgical goal is to repair or strengthen the valve between the bladder and ureter to prevent urine from flowing backward.
Surgical options include:
-
Open surgery – The most common approach to repair the faulty valve. The surgeon makes an incision in the lower abdomen and reconstructs the valve. After surgery, a catheter remains in place for a few days to help drain urine. Recovery typically requires a short hospital stay.
-
Robot-assisted laparoscopic surgery – A minimally invasive surgery using small incisions and robotic arms for precision. This method usually results in less bladder irritation and smaller scars, though it may have a slightly higher risk of complications such as urine leakage.
-
Endoscopic surgery – A minimally invasive procedure where a cystoscope is inserted through the urethra. The surgeon injects a special gel around the ureter’s opening to improve valve function. This is an outpatient surgery, meaning the child can often go home the same day. However, success rates may be slightly lower than with open surgery.
-
Nephrectomy – In rare and severe cases, when a kidney is severely damaged or infected and not functioning well, partial or total removal of the affected kidney may be necessary.
Comprehensive Care
Treatment for vesicoureteral reflux often includes addressing related conditions such as bowel or bladder dysfunction. Specialized pelvic floor rehabilitation and biofeedback programs can help children with recurring urinary tract infections or bladder control issues.
When surgery is required, modern surgical techniques such as the hidden incision endoscopic surgery (HIdES) procedure allow for effective correction with minimal visible scarring, ensuring the best outcomes with the least invasive approach.
Advertisement