Overview
Diagnosis
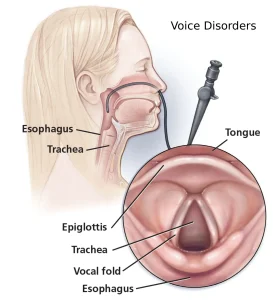
To diagnose a voice disorder, your healthcare provider will begin by asking about your voice problems and performing a thorough examination. You may be given a numbing medicine before the procedure to make it more comfortable. Several tools and tests may be used during diagnosis, including:
-
Mirror: A small, angled mirror similar to a dental mirror is placed into the mouth to view the vocal cords.
-
Flexible laryngoscope: A thin, bendable tube with a light and camera is inserted through the nose to examine the vocal cords.
-
Rigid laryngoscope: This stiff viewing tube is inserted through the mouth to get a clearer, more detailed view.
-
Videostroboscope: A camera combined with a flashing light captures slow-motion video of the vocal cords as they move, helping detect abnormalities in vibration and movement.
Additional diagnostic tests may include:
-
Sound analysis: Using computer software, this test measures irregularities or changes in sound produced by the vocal cords.
-
Laryngeal electromyography (EMG): Small needles inserted through the skin measure electrical currents in the muscles of the voice box to assess muscle and nerve function.
Treatment
Treatment for voice disorders depends on the specific diagnosis and the underlying cause. Options may include lifestyle changes, medications, voice therapy, or surgical procedures.
-
Rest, hydration, and voice therapy: Proper rest and adequate fluid intake help maintain healthy vocal cords. Speech-language pathologists teach techniques for efficient voice use, throat clearing, and proper hydration.
-
Allergy management: If allergies cause throat mucus buildup, treating the allergy can help improve voice quality.
-
Smoking cessation: Quitting smoking improves vocal health, boosts heart health, and reduces the risk of cancer and other diseases.
-
Medications: Depending on the cause, medications can reduce inflammation, treat reflux, or stop abnormal blood vessel growth. These may be taken orally, injected into the vocal cords, or applied directly during surgery.
Procedures
For more severe or persistent voice disorders, surgical or minimally invasive procedures may be necessary.
-
Removal of growths: Noncancerous growths on the vocal cords can be removed using microsurgery, carbon-dioxide laser surgery, or potassium titanyl phosphate (KTP) laser treatment. KTP laser therapy targets the blood supply to the lesion, allowing removal while preserving healthy tissue.
-
Injections: Tiny doses of botulinum toxin injected into neck muscles can reduce spasms or abnormal muscle movements. This treatment is particularly effective for spasmodic dysphonia, a neurological condition that affects vocal muscle control.
If one vocal cord is paralyzed and does not move, it can cause hoarseness or choking when swallowing liquids. The condition may improve naturally, but if it does not, procedures to move the paralyzed vocal cord closer to the middle of the windpipe may be recommended. These include:
-
Fat or collagen injection: Injecting body fat or synthetic collagen adds volume to the paralyzed vocal cord, helping it move closer to the center and improving voice strength.
-
Thyroplasty: A small opening is made in the cartilage of the voice box, and an implant is placed to push the paralyzed vocal cord toward the middle. This helps the vocal cords meet and vibrate effectively, improving voice quality and swallowing function.
Advertisement