Overview
Diagnosis and testing
To diagnose ulcerative colitis, healthcare professionals typically perform a colonoscopy and take small tissue samples, called biopsies, from the lining of the colon. These tests help confirm inflammation and rule out other forms of inflammatory bowel disease, such as Crohn’s disease. Additional tests like stool analysis, MRI, or CT scans may be used to detect complications and assess the extent of the condition.
To manage ulcerative colitis effectively, several tests and procedures may be recommended based on your symptoms and medical history.
Lab tests
-
Blood tests: These check for anemia, which occurs when there aren’t enough red blood cells to carry oxygen, and for signs of infection or inflammation.
-
Stool studies: These tests detect white blood cells or certain proteins in stool that indicate inflammation. Stool samples can also help rule out bacterial, viral, or parasitic infections.
Endoscopic procedures
-
Colonoscopy: This procedure uses a thin, flexible tube with a camera to view the entire colon. Tissue samples are taken for biopsy, which is necessary to confirm the diagnosis.
-
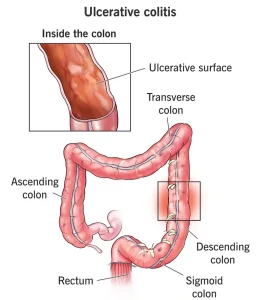
Flexible sigmoidoscopy: Similar to colonoscopy but using a shorter tube, this test examines the rectum and sigmoid colon. It’s often used when inflammation is too severe for a full colonoscopy.
Imaging procedures
-
X-ray: A standard abdominal X-ray can help rule out colon dilation, a serious complication that can lead to toxic megacolon or perforation.
-
CT scan: A CT scan of the abdomen or pelvis helps detect inflammation or abscesses that may cause pain.
-
CT enterography and MR enterography: These noninvasive tests are more sensitive for detecting inflammation in the small intestine. MR enterography is a radiation-free option.
Treatment
Ulcerative colitis treatment focuses on controlling inflammation, managing symptoms, and preventing flare-ups. Treatment options include medicines and, in severe cases, surgery. Since people respond differently to medications, it can take time to find the most effective treatment plan.
Anti-inflammatory medicines
These are usually the first step in treating ulcerative colitis.
-
Oral 5-aminosalicylates: Examples include sulfasalazine, mesalamine, and balsalazide. These medicines reduce inflammation and are often used long-term to maintain remission.
-
Corticosteroids: Prednisone and budesonide are used for moderate to severe cases that don’t respond to other treatments. They are effective for short-term control but are not safe for long-term use.
Immunomodulators
These medicines suppress the immune system to reduce inflammation.
-
Azathioprine and mercaptopurine: Commonly used immunomodulators that require regular blood monitoring due to potential side effects on the liver or pancreas.
Biologic medicines
Biologics target specific proteins in the immune system to reduce inflammation.
-
TNF inhibitors: Infliximab, adalimumab, and golimumab help people with severe ulcerative colitis who don’t respond to standard treatments.
-
Vedolizumab: Blocks inflammatory cells from reaching the colon.
-
Ustekinumab, mirikizumab, risankizumab, and guselkumab: These biologics target proteins involved in inflammation and are options for people who cannot tolerate other treatments.
Small molecule medicines
These oral treatments reduce inflammation by targeting specific immune pathways.
-
JAK inhibitors: Tofacitinib and upadacitinib control intestinal inflammation.
-
S1P receptor modulators: Ozanimod and etrasimod help reduce inflammation through immune system regulation.
Other medicines
Additional medicines may be prescribed to manage specific symptoms.
-
Antidiarrheal medicines: Loperamide may help with severe diarrhea but should be used with caution.
-
Pain relievers: Acetaminophen is preferred, while NSAIDs like ibuprofen and naproxen should be avoided as they can worsen symptoms.
-
Antispasmodics: These help relieve abdominal cramping.
-
Iron supplements: Used to treat iron deficiency anemia caused by intestinal bleeding.
Surgery
Surgery may be necessary if medicines fail or cause severe side effects, or if complications such as bleeding or colon cancer occur. The main surgical procedure is a proctocolectomy, which removes the entire colon and rectum, curing ulcerative colitis.
Types of surgical approaches include:
-
Ileoanal anastomosis (J-pouch): Creates a pouch from the small intestine attached to the anus, allowing for normal waste elimination.
-
Permanent ileal stoma: Involves creating an opening in the abdomen for stool to pass into a collection bag.
-
Continent ileostomy (Kock pouch): Uses a one-way valve that allows controlled stool drainage with a tube.
Cancer surveillance
People with ulcerative colitis are at higher risk of colon cancer and require regular screenings.
-
Those with inflammation beyond the rectum should have colonoscopies every 1 to 2 years, starting eight years after diagnosis.
-
The frequency depends on the level and duration of inflammation.
-
People with proctitis only are not at increased cancer risk.
Regular follow-up and personalized treatment can help manage symptoms effectively and reduce complications associated with ulcerative colitis.
Advertisement