Overview
Diagnosis
It’s important to determine the type of urinary incontinence you have, as your symptoms often guide the diagnosis and treatment plan. Your doctor will begin with a detailed medical history and physical examination. You may also be asked to perform a simple maneuver, such as coughing, to demonstrate incontinence.
Common diagnostic tests and evaluations include:
-
Urinalysis: Checks a urine sample for signs of infection, blood, or other abnormalities.
-
Bladder diary: For several days, you record fluid intake, frequency of urination, amount of urine passed, and any incontinence episodes.
-
Postvoid residual measurement: After urinating, your doctor measures how much urine remains in your bladder using a catheter or ultrasound. A significant amount of leftover urine may indicate a blockage or nerve or muscle problem in the bladder.
If more information is needed, your doctor may recommend additional tests such as urodynamic studies or pelvic ultrasound. These more-detailed evaluations are often suggested if surgery is being considered.
Treatment
Treatment for urinary incontinence depends on the type, severity, and underlying cause of the condition. Often, a combination of approaches is used. If a related medical condition is causing symptoms, that issue is treated first. Doctors usually begin with less invasive options before considering advanced therapies or surgery.
Behavioral Techniques
These methods are often the first line of treatment:
-
Bladder training: Delaying urination for a set period after feeling the urge, gradually increasing the time between bathroom trips to every 2.5–3.5 hours.
-
Double voiding: Urinating, then waiting a few minutes before trying again to help empty the bladder more completely.
-
Scheduled toilet trips: Going to the bathroom every two to four hours rather than waiting for the urge.
-
Fluid and diet management: Reducing or avoiding caffeine, alcohol, and acidic foods. Maintaining a healthy weight and adjusting fluid intake can also help improve bladder control.
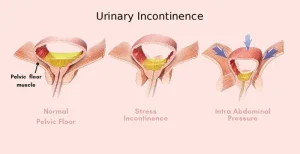
Pelvic Floor Muscle Exercises
Also known as Kegel exercises, these strengthen the muscles that control urination and are especially useful for stress incontinence.
How to perform them:
-
Tighten the muscles used to stop urination and hold for five seconds, then relax for five seconds.
-
Gradually increase to holding contractions for 10 seconds at a time.
-
Aim for three sets of 10 repetitions daily.
A pelvic floor physical therapist or biofeedback may help identify and strengthen the correct muscles.
Medications
Medications can help reduce or eliminate incontinence symptoms depending on the cause.
Common options include:
-
Anticholinergics: Calm an overactive bladder (oxybutynin, tolterodine, darifenacin, fesoterodine, solifenacin, trospium chloride).
-
Mirabegron (Myrbetriq): Relaxes the bladder muscle and increases bladder capacity for urge incontinence.
-
Alpha blockers: Used in men to relax the bladder neck and prostate muscles, making it easier to urinate (tamsulosin, alfuzosin, silodosin, doxazosin).
-
Topical estrogen: Low-dose vaginal cream, ring, or patch to strengthen tissues in the urethra and vaginal area.
Electrical Stimulation
Temporary electrodes are inserted into the rectum or vagina to stimulate and strengthen the pelvic floor muscles. This gentle electrical stimulation can benefit both stress and urge incontinence but usually requires multiple treatments over several months.
Medical Devices
Devices for women with incontinence include:
-
Urethral insert: A small, disposable device inserted into the urethra before activities that trigger leakage, such as exercise.
-
Pessary: A flexible silicone ring worn inside the vagina to support the urethra and prevent leakage.
Interventional Therapies
For persistent symptoms, doctors may recommend procedures such as:
-
Bulking material injections: A synthetic material injected around the urethra to help it stay closed. Often used for stress incontinence.
-
OnabotulinumtoxinA (Botox): Injected into the bladder muscle to relax it and control urge incontinence. Used when other treatments fail.
-
Nerve stimulators: Devices that deliver mild electrical pulses to the sacral nerves involved in bladder control. These can be implanted or temporarily inserted and are effective for overactive bladder and urge incontinence.
Surgery
If other treatments do not provide relief, surgical options may be considered:
-
Sling procedures: Synthetic mesh or tissue from your own body creates a sling under the urethra to keep it closed during pressure activities such as coughing or sneezing.
-
Bladder neck suspension: Provides support to the urethra and bladder neck through an abdominal incision.
-
Prolapse surgery: For women with both pelvic organ prolapse and incontinence, combining sling and prolapse repair may be recommended.
-
Artificial urinary sphincter: A small device implanted around the bladder neck that can be manually controlled to release urine.
Absorbent Pads and Catheters
If incontinence cannot be fully managed with medical treatment, practical aids can help maintain comfort and quality of life.
-
Pads and protective garments: Modern options are discreet and comfortable for daily wear. Men may use drip collectors for minor leakage.
-
Catheters: For those unable to empty their bladder completely, intermittent self-catheterization may be recommended. Your doctor will provide guidance on safe cleaning and use.
This approach ensures a comprehensive and individualized treatment plan for managing urinary incontinence effectively.
Advertisement