Overview
Diagnosis of Barrett’s Esophagus
Barrett’s esophagus is diagnosed primarily using endoscopy and biopsy to assess abnormal changes in the esophageal lining:
-
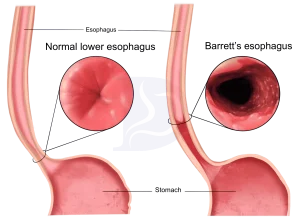
Endoscopy: A lighted tube with a camera (endoscope) is passed through the throat to examine the esophagus. Normal esophagus tissue appears pale and glossy, while Barrett’s tissue looks red and velvety.
-
Biopsy: Tissue samples are removed from the esophagus to examine for cellular changes.
-
Pathology assessment: A pathologist evaluates the tissue for dysplasia, which indicates precancerous changes:
-
No dysplasia: Barrett’s tissue is present but no precancerous changes are found.
-
Low-grade dysplasia: Early precancerous changes are detected in the cells.
-
High-grade dysplasia: Advanced precancerous changes, considered a step before potential esophageal cancer.
-
Screening recommendations
Men with chronic GERD symptoms, especially those over 50 or with additional risk factors (family history, smoking, abdominal obesity, or being white), may be recommended for screening. Women with uncontrolled reflux or other risk factors may also be screened.
Treatment of Barrett’s Esophagus
Treatment depends on the degree of dysplasia and overall patient health:
-
No dysplasia:
-
Periodic endoscopy to monitor the esophagus, typically every one to five years depending on initial findings.
-
Management of GERD with medications, lifestyle changes, or surgical procedures such as hiatal hernia repair or lower esophageal sphincter tightening.
-
-
Low-grade dysplasia:
-
Confirm diagnosis with an experienced pathologist.
-
Follow-up endoscopy every six to twelve months.
-
Endoscopic treatments may include:
-
Endoscopic resection to remove damaged tissue.
-
Radiofrequency ablation to destroy abnormal cells using heat.
-
Cryotherapy, which uses cycles of freezing and thawing to damage abnormal cells.
-
-
Additional acid-suppressing therapy may be used before re-evaluation.
-
-
High-grade dysplasia:
-
Considered a precursor to esophageal cancer.
-
Treatment options include endoscopic resection, radiofrequency ablation, cryotherapy, or surgical removal of the affected esophagus with reconstruction.
-
Lifelong acid-reducing therapy may be recommended after non-surgical treatments to support healing and prevent recurrence.
-
Regular follow-up is essential as Barrett’s esophagus can recur, and monitoring helps prevent progression to esophageal cancer.
High-grade dysplasia
High-grade dysplasia is generally thought to be a precursor to esophageal cancer. For this reason, your doctor may recommend endoscopic resection, radiofrequency ablation or cryotherapy. Another option may be surgery, which involves removing the damaged part of your esophagus and attaching the remaining portion to your stomach.
Recurrence of Barrett’s esophagus is possible after treatment. Ask your doctor how often you need to come back for follow-up testing. If you have treatment other than surgery to remove abnormal esophageal tissue, your doctor is likely to recommend lifelong medication to reduce acid and help your esophagus heal.
Advertisement