Overview
Diagnosis
To diagnose cholangiocarcinoma (bile duct cancer), your doctor may recommend several tests based on your symptoms and overall health.
Liver function tests help measure how well your liver is working and provide clues about possible bile duct issues.
Tumor marker testing measures levels of carbohydrate antigen (CA) 19-9, a protein often produced in excess by bile duct cancer cells. However, elevated CA 19-9 levels do not always indicate cancer, as they can also be present in other bile duct conditions such as inflammation or obstruction.
Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure in which a thin, flexible tube with a camera is passed through your digestive tract to examine the bile ducts. Dye may be injected to make the bile ducts more visible during imaging.
Imaging tests, including ultrasound, CT scans, MRI, and magnetic resonance cholangiopancreatography (MRCP), help visualize internal organs and identify signs of bile duct cancer. MRCP provides detailed 3D images without the need for injected dye and is often used as a noninvasive alternative to ERCP.
A biopsy may be performed to collect a small tissue sample for microscopic analysis. The method depends on the tumor’s location. If near the small intestine, the sample can be collected during ERCP. If near or within the liver, a fine-needle aspiration guided by imaging may be used.
It’s important to discuss biopsy options carefully, as certain techniques can affect future treatment eligibility, such as liver transplantation. Once diagnosed, staging tests help determine the extent of cancer and guide treatment planning.
Treatment
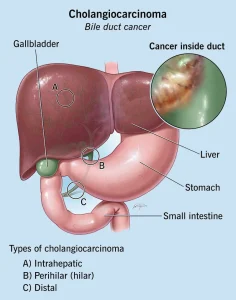
Treatment for cholangiocarcinoma depends on the cancer’s stage, location, and whether it can be surgically removed.
Surgery is the primary option when the tumor can be removed completely. For small cancers, part of the bile duct may be removed and reconnected. More advanced cases may require removing portions of the liver, pancreas, or lymph nodes.
Liver transplant surgery may be an option for selected patients with hilar cholangiocarcinoma. This approach can be curative but carries a risk of recurrence after transplantation.
Chemotherapy uses drugs to destroy cancer cells. It can be administered before a liver transplant or to control advanced cancer. Drugs may be given intravenously or targeted directly to cancerous tissue.
Radiation therapy uses high-energy beams, such as X-rays or protons, to destroy cancer cells. This may involve external beam radiation or internal brachytherapy, where radioactive material is placed near the tumor.
Targeted drug therapy focuses on specific genetic or molecular changes in cancer cells. Testing can determine if your cholangiocarcinoma may respond to targeted treatments.
Immunotherapy boosts your immune system to help fight cancer. It can be effective in advanced cases when other treatments are not successful.
Radiofrequency ablation destroys cancer cells using heat generated by electrical currents delivered through thin needles guided by imaging.
Photodynamic therapy involves injecting a light-sensitive drug that accumulates in cancer cells. When exposed to laser light, the drug activates and kills these cells. This method may relieve symptoms and slow cancer progression, though multiple treatments are usually needed.
Biliary drainage helps restore bile flow by inserting stents or performing bypass surgery. This can relieve symptoms such as jaundice and improve comfort.
Because cholangiocarcinoma is complex and challenging to treat, it’s important to seek care from experienced specialists or get a second opinion.
Clinical Trials
Clinical trials test new treatments, including innovative drugs, surgical methods, or combined therapies. While participation doesn’t guarantee a cure, it can provide access to advanced treatments and contribute to medical research. Clinical trials are closely monitored for safety and effectiveness.
Ask your doctor if participating in a clinical trial might be suitable for your condition.
Supportive (Palliative) Care
Palliative care focuses on improving quality of life by managing symptoms such as pain, fatigue, and discomfort. It is provided alongside standard cancer treatments.
A team of palliative care professionals — including doctors, nurses, and therapists — works with your oncology team to offer comprehensive support for you and your family. This care can begin at any stage of your illness and may help patients feel better and live longer.
Palliative care is different from hospice or end-of-life care; it is an integral part of ongoing treatment for people living with serious conditions such as cholangiocarcinoma.
Advertisement