Overview
Diagnosis
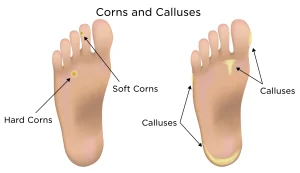
Your healthcare provider will likely diagnose corns and calluses by examining your feet. This examination helps rule out other causes of thickened skin, such as warts and cysts. To confirm the diagnosis, your provider may gently pare away a small portion of the hardened skin.
-
If the area bleeds or shows black dots (dried blood), it indicates a wart, not a corn.
-
If no bleeding or dark spots appear, it confirms a corn or callus.
Treatment
Treatment for corns and calluses is usually the same and focuses on removing the source of friction or pressure that caused them to develop. Wearing properly fitted shoes and using protective padding can significantly help.
If self-care measures don’t relieve discomfort, your healthcare provider may recommend one or more of the following medical treatments:
-
Trimming away excess skin
Your healthcare provider can safely remove thickened skin or trim a large corn using a scalpel during an office visit.
⚠️ Do not attempt this at home, as it can cause infection or injury. -
Medicated patches
Your provider may apply a patch containing 40% salicylic acid (brands like Clear Away, MediPlast, etc.). These are also available over the counter.-
Your provider will advise how often to replace the patch.
-
Before applying a new one, gently thin the thickened skin using a pumice stone, nail file, or emery board.
For larger areas, nonprescription salicylic acid gel (Compound W, Keralyt) or liquid forms (Compound W, Duofilm) can be used.
-
-
Shoe inserts (orthotics)
If a foot deformity is causing recurring pressure, your provider may prescribe custom-made padded shoe inserts to prevent future corns or calluses. -
Surgery
In some cases, surgery may be needed to correct bone alignment that leads to constant friction.
This is typically a minor procedure and can be done without an overnight hospital stay.
Advertisement