Overview
Diagnosis
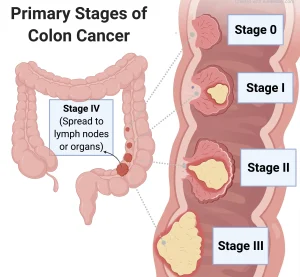
Colon cancer diagnosis often begins with a colonoscopy. This test may be done as part of a routine colon cancer screening or if you have symptoms that suggest a problem. If the colonoscopy shows something unusual, additional tests are performed to confirm the diagnosis and determine how far the cancer has spread — a process known as staging. Colon cancer stages range from stage 0 to stage 4.
Colon Cancer Screening Tests
Screening tests look for colon cancer in people without symptoms. Most adults at average risk should begin screening at age 45. Those with higher risk — due to family history or genetic conditions — may need to start earlier.
Types of screening tests include:
-
Colonoscopy:
A flexible tube with a camera is inserted into the rectum to examine the entire colon.-
Doctors can remove polyps or take biopsies during the same procedure.
-
This test is both diagnostic and therapeutic since removing precancerous polyps lowers the risk of colon cancer.
“A colonoscopy is not just diagnostic but can also be therapeutic. By removing the highly aggressive polyps, or at-risk polyps, you’ve technically removed the risk of colon cancer.”
— Tanios S. Bekaii-Saab, M.D., Mayo Clinic Oncologist -
-
Biopsy:
A tissue sample is collected, usually during a colonoscopy, and sent to a lab. Testing determines:-
Whether the cells are cancerous
-
How fast they are growing
-
Specific cell features that guide treatment planning
-
-
Stool Tests:
These noninvasive tests can be done at home and are best for people at average risk.-
Fecal Occult Blood Test (FOBT): Detects hidden blood in the stool. Two common types are:
-
gFOBT (guaiac-based test)
-
FIT (fecal immunochemical test)
Recommended once a year; about 90% effective when done regularly.
-
-
Stool DNA Test (e.g., Cologuard): Detects DNA changes linked to colon cancer.
-
Recommended every 1–3 years.
-
About 90% effective when performed annually.
-
⚠️ If any stool test is positive, a follow-up colonoscopy is required to confirm findings and remove polyps.
-
Other Diagnostic Tests
-
Shield Liquid Biopsy:
A new FDA-approved blood test that detects DNA changes linked to colon cancer or precancerous growths.-
Best for people at average risk.
-
Detected 83% of colon cancers in studies but only 13% of precancerous lesions.
-
-
Imaging Tests:
Imaging tests help determine how far the cancer has spread (staging) and include:-
CT scan – to check for tumors or metastasis.
-
MRI – especially for rectal cancer staging.
-
PET scan – to identify cancer activity in other organs.
-
Genetic Testing
While not used to diagnose colon cancer, genetic testing helps identify hereditary risk factors and can guide both treatment and family screening.
Genetic testing may be recommended if you:
-
Have a strong family history of colon cancer or multiple polyps.
-
Have colon cancer and another type of cancer.
-
Have a family history of Lynch syndrome, familial adenomatous polyposis (FAP), or MUTYH-associated polyposis (MAP).
-
Have relatives with colon, rectal, uterine, or endometrial cancer.
-
Were diagnosed before age 50.
In summary:
Diagnosis of colon cancer involves a combination of screening (colonoscopy, stool tests, blood tests) and staging (imaging and biopsy) to understand the cancer’s type, extent, and behavior. Genetic testing provides additional insight into inherited risk and helps tailor prevention and treatment plans.
Advertisement