Overview
Diagnosis
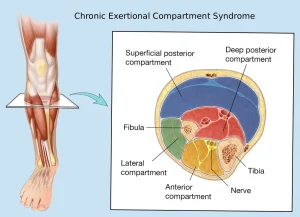
Chronic exertional compartment syndrome can be challenging to diagnose because its symptoms resemble other exercise-related conditions such as shin splints or stress fractures. Your doctor will first rule out these more common causes before recommending specialized tests.
A physical exam may not reveal any issues at rest. However, your doctor might examine you after you exercise to the point where symptoms appear. At that time, muscle bulging, tenderness, or tension in the affected area may be visible.
Imaging Studies
Imaging tests can help evaluate muscle structure, blood flow, and possible alternative causes of pain. These may include:
Magnetic Resonance Imaging (MRI)
A standard MRI of your legs helps assess muscle structure and rule out other conditions.
An advanced MRI can measure fluid volumes within muscle compartments. Images are taken before exercise, during movement when symptoms appear, and after exercise. This method is accurate for detecting CECS and may reduce the need for invasive pressure testing.
Near Infrared Spectroscopy (NIRS)
NIRS is a newer, noninvasive technique that measures blood oxygen levels in the affected muscle tissue. It’s done both at rest and after exercise to determine if blood flow is restricted within the muscle compartments.
Compartment Pressure Testing
If imaging does not show a clear cause, your doctor may recommend compartment pressure measurement — the gold standard for diagnosing CECS.
This test involves inserting a needle or catheter into the muscle before and after exercise to measure internal pressure. Because the procedure is invasive and mildly painful, it’s typically performed only when other tests strongly suggest CECS.
Treatment
Treatment options for chronic exertional compartment syndrome include both nonsurgical and surgical approaches.
Nonsurgical Options
Initial management may include:
-
Pain relief medications
-
Physical therapy
-
Orthotic shoe inserts
-
Massage therapy
-
Rest or reducing the intensity of the triggering activity
Adjusting your running or walking technique, such as changing how your feet strike the ground, may also help. However, nonsurgical treatments often provide only temporary relief for true CECS.
In some cases, injections of botulinum toxin A (Botox) into the affected muscles may reduce symptoms. More research is needed to confirm its effectiveness.
Surgical Options
The most effective treatment for CECS is a fasciotomy — a surgical procedure that involves cutting the fascia (the tough tissue surrounding muscle compartments) to relieve pressure.
Some fasciotomies can be performed using small incisions, which may shorten recovery time and allow an earlier return to sports or physical activity.
Although most people experience improvement, surgery carries risks such as infection, nerve injury, numbness, weakness, bruising, or scarring.
Self-Care
To help manage pain and reduce symptoms:
-
Use proper athletic shoes or orthotics.
-
Switch to low-impact exercises such as cycling, swimming, or using an elliptical trainer.
-
Stretch the affected limb after exercise.
-
Avoid activities that cause pain until recovery is complete.
Preparing for Your Appointment
You may start by seeing your family doctor, who might refer you to a specialist in sports medicine or orthopedic surgery.
What You Can Do
When scheduling your appointment, ask if you need to prepare in advance. Bring a list of:
-
Your symptoms, including when they occur and what triggers them
-
Your activity level, sports involvement, and exercise routine
-
All medications and supplements you take, including dosages
If possible, bring copies of any recent imaging results. You may also bring a family member or friend to help you remember details discussed during the appointment.
Questions to Ask Your Doctor
-
What is the most likely cause of my symptoms?
-
What tests do I need?
-
Is my condition temporary or chronic?
-
What treatment options do you recommend?
-
Are there any activity restrictions I should follow?
-
Should I see a specialist?
-
Where can I find reliable information about this condition?
What to Expect from Your Doctor
Your doctor may ask questions such as:
-
When did your symptoms begin?
-
Do your symptoms occur continuously or intermittently?
-
What activities trigger your pain?
-
How long does it take for your symptoms to ease after stopping exercise?
-
Do you experience weakness, numbness, or tingling in your legs or feet?
Advertisement