Overview
Diagnosis
Diagnosing kidney disease begins with a detailed discussion of your personal and family medical history. Your doctor may ask if you have high blood pressure, take medications that could affect kidney function, have noticed any changes in urination, or have family members with kidney disease.
A physical exam is then performed to check for signs of heart or blood vessel issues, and sometimes a neurological exam is included.
To confirm the diagnosis and determine how advanced the kidney disease is, you may need one or more of the following tests:
-
Blood tests: These measure levels of waste products, such as creatinine and urea, to assess how well your kidneys are functioning.
-
Urine tests: Examining a urine sample can detect abnormalities that suggest chronic kidney failure and help identify the cause.
-
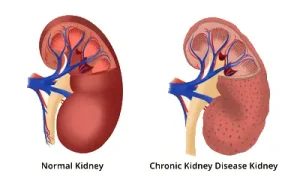
Imaging tests: Ultrasound or other imaging scans can reveal changes in the size or structure of your kidneys.
-
Kidney biopsy: In some cases, a small sample of kidney tissue is removed using a thin needle under local anesthesia. The sample is sent to a lab to help determine the cause of kidney damage.
Treatment
While some types of kidney disease can be treated, chronic kidney disease often has no cure. Treatment focuses on managing symptoms, preventing complications, and slowing disease progression. In severe cases, treatment for end-stage kidney disease may be necessary.
Treating the cause
Your doctor will work to manage or control the underlying cause of your kidney disease. Treatment varies depending on the condition — for example, controlling blood sugar in diabetes or lowering blood pressure in hypertension. However, kidney damage can continue to progress even if the underlying issue is well managed.
Treating complications
Managing complications helps improve comfort and quality of life. Treatments may include:
-
High blood pressure medications: Angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) can lower blood pressure and help protect kidney function. Your doctor may also recommend a diuretic and a low-salt diet.
-
Medications to relieve swelling: Diuretics help remove excess fluid from the body and reduce swelling and high blood pressure.
-
Medications to treat anemia: Erythropoietin supplements, sometimes combined with iron, help the body produce more red blood cells, easing fatigue and weakness.
-
Cholesterol-lowering medications: Statins help reduce high cholesterol, which is common in kidney disease and increases heart disease risk.
-
Bone-protecting medications: Calcium and vitamin D supplements, along with phosphate binders, help prevent weak bones and reduce calcium buildup in blood vessels.
-
Dietary changes: A lower-protein diet may be recommended to reduce waste buildup in the blood. A registered dietitian can help plan a balanced, kidney-friendly meal plan.
Regular monitoring helps your healthcare team track whether your condition is stable or progressing.
Treatment for end-stage kidney disease
If your kidneys can no longer filter waste and fluids effectively, you may develop end-stage kidney disease. At this stage, treatment options include dialysis or kidney transplant.
-
Dialysis: This procedure removes waste products and excess fluid from the blood.
-
Hemodialysis uses a machine to filter the blood.
-
Peritoneal dialysis uses a special fluid introduced into the abdomen to absorb waste before being drained.
-
-
Kidney transplant: A healthy kidney from a donor is surgically placed into your body. Transplants can come from living or deceased donors. Lifelong medication is needed to prevent organ rejection.
For those who do not pursue dialysis or transplant, conservative management is an option. This focuses on symptom control, advance care planning, and maintaining comfort through palliative care.
Advertisement