Overview
Diagnosis
Chronic obstructive pulmonary disease (COPD) can be difficult to diagnose because its symptoms often resemble those of other lung conditions. Many people are not diagnosed until the disease has already progressed.
To diagnose COPD, your healthcare professional reviews your symptoms, medical and family history, and exposure to lung irritants such as cigarette smoke. A physical exam is performed, including listening to your lungs. You may also have tests such as pulmonary function tests, lab tests, and imaging studies.
Pulmonary Function Tests
These tests measure how well your lungs are working and how efficiently air moves in and out.
-
Spirometry measures how much air your lungs can hold and how quickly you can exhale. It is the main test used to diagnose COPD and assess airflow limitation.
-
Lung volume testing measures how much air your lungs hold during inhalation and exhalation.
-
Lung diffusion testing checks how effectively oxygen and carbon dioxide move between your lungs and bloodstream.
-
Pulse oximetry measures the oxygen level in your blood using a small device placed on your finger. A six-minute walk test may also be done to check oxygen saturation during activity.
-
Exercise stress testing may be used to assess heart and lung function while you exercise on a treadmill or stationary bike.
Imaging
-
A chest X-ray may show signs of lung changes from COPD and can help rule out other conditions such as heart failure.
-
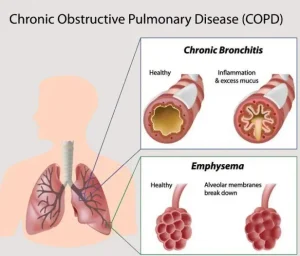
A CT scan provides detailed images of the lungs and can show emphysema and chronic bronchitis. It can also help determine if surgery may be beneficial and check for lung cancer.
These imaging and lung function tests are also used over time to monitor your condition and evaluate how well treatment is working.
Lab Tests
-
Arterial blood gas analysis measures how well your lungs move oxygen into your blood and remove carbon dioxide.
-
Testing for alpha-1-antitrypsin (AAT) deficiency identifies a genetic cause of COPD.
-
Other blood tests may help find the cause of your symptoms or rule out different conditions.
Treatment
Treatment depends on the severity of symptoms and how often you experience flare-ups, known as exacerbations. Proper management can control symptoms, slow disease progression, reduce complications, and improve quality of life.
Quitting Smoking
The most important step in COPD treatment is quitting smoking. Stopping smoking helps prevent further lung damage and improves breathing. Your healthcare professional can recommend:
-
Smoking cessation programs and support groups
-
Nicotine replacement products
-
Medications to reduce cravings and withdrawal symptoms
Avoiding secondhand smoke is also essential.
Medicines
Most COPD medications are delivered through inhalers, which allow the medicine to go directly into the lungs. Nebulizers, which turn liquid medicine into a mist, may also be used.
-
Bronchodilators relax the airway muscles and make breathing easier. Short-acting options include albuterol, ipratropium, and levalbuterol. Long-acting bronchodilators are used daily to maintain open airways.
-
Inhaled corticosteroids reduce inflammation and prevent flare-ups. They may cause mild side effects such as hoarseness or mouth infections.
-
Combination inhalers may include two bronchodilators or a bronchodilator plus a steroid. Common examples are Anoro Ellipta, Breztri Aerosphere, and Trelegy Ellipta.
-
Oral steroids are used for short periods during flare-ups but can have serious side effects if taken long term.
-
Phosphodiesterase-4 inhibitors, such as roflumilast, reduce inflammation and help prevent flare-ups in people with severe COPD and chronic bronchitis.
-
Theophylline may be prescribed when other treatments are not effective or affordable, but it requires regular blood monitoring due to possible side effects.
-
Antibiotics may be used during infections that worsen COPD symptoms. Long-term use may help prevent flare-ups but can lead to antibiotic resistance.
Therapies
-
Oxygen therapy may be prescribed if blood oxygen levels are low. Supplemental oxygen can be delivered through a mask or nasal tubing and may be used continuously or only during activity or sleep.
-
Pulmonary rehabilitation programs combine exercise, education, nutrition, and counseling to improve physical endurance and quality of life.
-
In-home noninvasive ventilation therapy, such as BiPAP, helps people with severe COPD breathe easier, particularly at night, and may reduce hospital visits.
Managing Flare-Ups
Exacerbations can last for days or weeks and may lead to serious complications if untreated. Triggers include respiratory infections, pollution, or other irritants. Seek medical attention if you notice:
-
Worsening cough
-
Increased mucus or change in its color
-
Greater difficulty breathing
Treatment may include antibiotics, steroids, oxygen, or hospitalization. Preventing future flare-ups involves:
-
Taking prescribed medications
-
Avoiding air pollution
-
Getting annual flu and pneumonia vaccines
-
Quitting smoking
Surgery
Surgical treatment may help people with severe COPD, especially when medication alone is not effective. Options include:
-
Lung volume reduction surgery, which removes damaged lung tissue to improve breathing.
-
Endoscopic lung volume reduction, a minimally invasive procedure that places a valve to collapse the most damaged lung area, allowing healthier parts to expand.
-
Lung transplant, which may improve breathing and activity levels but carries risks and requires lifelong medication.
-
Bullectomy, which removes large air sacs (bullae) that trap air and prevent proper lung function.
Alpha-1-Antitrypsin Deficiency
For people with COPD caused by AAT deficiency, treatment includes standard COPD management and replacement therapy with AAT protein to protect the lungs from further damage.
Advertisement