Overview
Diagnosis
To determine the cause of chronic pelvic pain, your healthcare team will ask detailed questions about your symptoms, medical history, and family health conditions. You may also be asked to keep a journal of your pain and other symptoms to help describe how the pain affects your daily life.
Common tests and exams include:
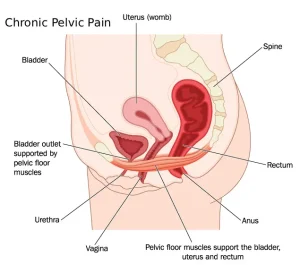
• Pelvic exam – This exam checks for signs of illnesses, growths, or tense pelvic floor muscles. Your healthcare professional will note any tender areas and stop if you feel discomfort.
• Lab tests – Blood, urine, or swab tests may be done to check for infections such as chlamydia, gonorrhea, or urinary tract infections.
• Ultrasound – This imaging test uses sound waves to create pictures of the pelvic organs and can detect growths or cysts in the uterus, ovaries, or fallopian tubes.
• Other imaging tests – CT scans or MRI may be used to detect structural issues or growths inside the body.
• Laparoscopy – A minor surgical procedure that uses a small camera inserted through a small cut in the abdomen to view pelvic organs. It helps diagnose and sometimes treat conditions such as endometriosis or chronic pelvic inflammatory disease.
Finding the exact cause of chronic pelvic pain can take time, and sometimes no clear reason is identified. Open communication with your healthcare team is important to develop a treatment plan that improves comfort and quality of life.
Treatment
The main goal of treatment for chronic pelvic pain is to relieve symptoms and enhance daily functioning. If a specific cause is identified, treatment targets that condition. Otherwise, care focuses on managing pain and improving quality of life through a combination of approaches.
Medications
Depending on the cause, medicines that may be used include:
• Pain relievers – Over-the-counter options such as ibuprofen, aspirin, or acetaminophen can ease discomfort. Stronger prescription medicines may be used for severe pain.
• Hormone treatments – Hormonal therapy, including birth control pills, may help reduce pain that occurs in cycles with menstruation.
• Antibiotics – Used when a bacterial infection is identified as the cause.
• Antidepressants – Certain antidepressants, such as amitriptyline, duloxetine, or venlafaxine, may relieve chronic pain even without depression.
• Muscle relaxers – Medicines like cyclobenzaprine may help ease muscle tension linked with pelvic pain.
Other therapies
Non-drug therapies may also provide relief for chronic pelvic pain.
• Physical therapy – Helps stretch and release tight muscles and tissues. Techniques may include myofascial release, transcutaneous electrical nerve stimulation, biofeedback, or dry needling.
• Spinal cord stimulation – Also known as neuromodulation, this procedure implants a device that blocks pain signals from reaching the brain.
• Trigger point injections – Injections of numbing medicine into tight, painful spots can help reduce discomfort.
• Talk therapy – Psychological counseling, including cognitive behavioral therapy or sex therapy, can help address emotional stress, anxiety, trauma, or relationship issues linked with pain.
Surgery
Surgery may be recommended if a treatable physical cause is found.
• Laparoscopy – Used to remove or treat endometriosis tissue and other painful lesions.
• Hysterectomy or oophorectomy – In rare cases, removal of the uterus and one or both ovaries may be considered. These surgeries have significant long-term effects, so benefits and risks should be carefully discussed.
Pain rehabilitation programs
Managing chronic pelvic pain may require a combination of medical, physical, and psychological therapies. A comprehensive pain rehabilitation program can help individuals find the right balance of treatments and coping strategies to improve daily life.
Advertisement