Overview
Diagnosis
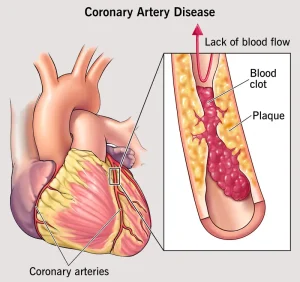
To diagnose coronary artery disease (CAD), your healthcare provider will examine you, review your medical history, and ask about any symptoms such as chest pain (angina) or shortness of breath. If CAD is suspected, several tests may be recommended to assess your heart’s function and blood flow.
Tests Used to Diagnose Coronary Artery Disease
-
Blood tests
These check for cholesterol, blood sugar, and high-sensitivity C-reactive protein (CRP) levels — a marker of artery inflammation. -
Electrocardiogram (ECG or EKG)
This quick and painless test records the electrical activity of the heart. It can show evidence of a current or past heart attack or abnormal heart rhythms. -
Echocardiogram
Uses sound waves (ultrasound) to create moving images of the heart, showing how well it pumps blood and identifying areas weakened by poor oxygen supply or previous heart damage. -
Exercise stress test
If symptoms occur during physical activity, this test monitors your heart while you walk on a treadmill or pedal a stationary bike. If you can’t exercise, medication may be given to simulate the effects of exercise on your heart. Sometimes, this test is combined with an echocardiogram. -
Nuclear stress test
Involves injecting a small amount of radioactive tracer to show blood flow to the heart at rest and during stress. It helps locate areas of poor circulation or heart damage. -
Heart CT scan
A computed tomography (CT) scan detects calcium deposits and blockages in coronary arteries. When a dye is used to enhance imaging, the test is called a CT coronary angiogram. -
Cardiac catheterization and angiogram
A thin tube (catheter) is inserted through a blood vessel in the wrist or groin and guided to the heart. Contrast dye is injected to visualize arteries on X-rays, helping locate blockages. Treatment, such as angioplasty or stent placement, may be performed during this procedure.
Treatment
Treatment for coronary artery disease focuses on improving blood flow to the heart and preventing future complications. Options include lifestyle changes, medications, and surgical procedures, depending on the severity of the disease.
Lifestyle Changes
-
Quit smoking
-
Follow a heart-healthy diet (low in saturated fat, cholesterol, and salt)
-
Exercise regularly
-
Maintain a healthy weight
-
Manage stress effectively
Medications
Your healthcare provider may prescribe one or more of the following:
-
Cholesterol-lowering medicines – such as statins, niacin, fibrates, or bile acid sequestrants to reduce plaque buildup.
-
Aspirin – helps prevent blood clots. However, daily use may cause stomach or intestinal bleeding; always consult your doctor before starting.
-
Beta blockers – slow the heart rate and lower blood pressure, reducing the risk of another heart attack.
-
Calcium channel blockers – used when beta blockers aren’t suitable; they help ease chest pain.
-
ACE inhibitors or ARBs – lower blood pressure and slow the progression of CAD.
-
Nitroglycerin – widens blood vessels to relieve or prevent chest pain; available as a pill, patch, or spray.
-
Ranolazine – helps control long-term chest pain, often used with or instead of beta blockers.
Surgical and Other Procedures
-
Coronary angioplasty and stent placement
A balloon-tipped catheter opens a blocked artery, and a stent (small wire mesh tube) is placed to keep it open. Some stents release medication to prevent re-narrowing. -
Coronary artery bypass graft (CABG) surgery
Involves taking a healthy blood vessel from another part of the body and creating a new path for blood flow around blocked arteries. This improves blood supply to the heart muscle.
After surgery, cardiac rehabilitation may be recommended. This program combines exercise, education, and counseling to help you recover, strengthen your heart, and prevent future heart problems.
Advertisement