Overview
Diagnosis
Diagnosing cyclothymia (cyclothymic disorder) involves ruling out other mental health and medical conditions that may cause similar symptoms, such as bipolar I or II disorder, major depression, or thyroid problems.
To identify the right diagnosis, your healthcare provider may recommend the following:
-
Physical exam:
A thorough physical examination and lab tests are done to check for any underlying medical conditions that might be causing mood changes. -
Psychological evaluation:
A psychiatrist or mental health professional will discuss your thoughts, emotions, and behavior patterns. You may also complete psychological questionnaires, and—with your consent—family members or close friends may be interviewed to describe your symptoms, such as periods of hypomania or depression. -
Mood charting:
You may be asked to keep a daily log of your moods, sleep patterns, and other lifestyle factors. This helps your provider identify recurring emotional patterns and triggers.
Diagnostic Criteria
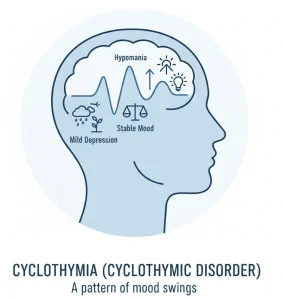
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association, cyclothymia is diagnosed when:
-
There have been many episodes of elevated mood (hypomanic symptoms) and depressive symptoms for at least two years (or one year in children and adolescents).
-
Periods of stable mood typically last less than two months.
-
Symptoms cause significant impairment in social, work, school, or personal life.
-
Symptoms do not meet the criteria for bipolar I or II disorder, major depressive disorder, or another mental condition.
-
Symptoms are not caused by substance use or a medical condition.
Treatment
Cyclothymia is a chronic condition that requires lifelong management, even during symptom-free periods. Treatment aims to:
-
Lower the risk of developing bipolar I or II disorder.
-
Stabilize mood fluctuations and reduce the intensity of emotional highs and lows.
-
Prevent relapse by maintaining consistent treatment.
-
Address substance use problems, which can worsen symptoms.
Medications
Although there are no FDA-approved drugs specifically for cyclothymia, your healthcare provider may prescribe medications used for bipolar disorder, such as:
-
Mood stabilizers to control hypomanic and depressive swings.
-
Antidepressants, used carefully, as they may sometimes trigger mood elevation.
-
Antipsychotic medicines, if mood stabilizers alone are not effective.
Medication plans are individualized and closely monitored to ensure safety and effectiveness.
Psychotherapy
Psychotherapy (talk therapy) is an essential part of managing cyclothymia. It helps you understand your emotions, develop coping strategies, and maintain stable daily routines.
Common therapy options include:
-
Cognitive Behavioral Therapy (CBT):
Focuses on recognizing and changing negative thinking patterns and behaviors. CBT also helps identify triggers and build stress management skills. -
Interpersonal and Social Rhythm Therapy (IPSRT):
Emphasizes regular daily routines—including sleep, meals, and exercise—to improve emotional stability and reduce mood swings. -
Other therapies:
Group therapy, mindfulness-based therapy, or family therapy may also be recommended, depending on your needs and lifestyle.
Advertisement