Overview
Depersonalization-Derealization Disorder is a mental health condition characterized by persistent or recurrent feelings of detachment from one’s self, surroundings, or both, while reality testing remains intact. Individuals may feel as if they are observing themselves from outside their body or that the world around them is unreal, dreamlike, or distorted. Despite these experiences, people with this disorder are aware that their perceptions are not real, which distinguishes it from psychotic disorders.
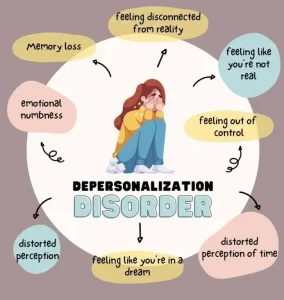
Symptoms
Symptoms may vary in intensity and can be continuous or episodic:
-
Feeling detached from one’s thoughts, emotions, or body
-
Sensation of being an outside observer of oneself
-
Emotional or physical numbness
-
Altered perception of time, space, or distance
-
Surroundings appearing flat, unreal, or visually distorted
-
Heightened self-awareness or anxiety about symptoms
-
Intact awareness that experiences are subjective and not real
Causes
The exact cause is not fully understood, but several factors may contribute:
-
Severe or prolonged stress
-
Anxiety disorders, especially panic disorder
-
Depression
-
Traumatic experiences or emotional abuse
-
Substance use, particularly cannabis or hallucinogens
-
Neurological or biochemical changes affecting perception
Risk Factors
Certain factors increase the likelihood of developing this disorder:
-
Adolescence or young adulthood
-
History of anxiety or depressive disorders
-
Exposure to traumatic or highly stressful events
-
Chronic stress or emotional instability
-
Use of psychoactive substances
-
Personality traits linked to high sensitivity or emotional reactivity
Complications
If left untreated, depersonalization-derealization disorder may lead to:
-
Persistent anxiety or panic attacks
-
Depression and emotional distress
-
Difficulty concentrating or functioning at work or school
-
Social withdrawal
-
Reduced quality of life
-
Increased health-related anxiety
Prevention
While not all cases can be prevented, certain measures may reduce risk or severity:
-
Early management of anxiety and stress
-
Seeking help after traumatic experiences
-
Avoiding recreational drug use
-
Maintaining healthy sleep and daily routines
-
Practicing stress-reduction techniques such as mindfulness
-
Seeking mental health support when symptoms first appear
Advertisement