Overview
Diagnosis
Gestational diabetes is usually diagnosed during the second trimester of pregnancy, typically between 24 and 28 weeks. However, if you’re at high risk, your healthcare professional may recommend testing earlier — sometimes at the first prenatal visit.
You may be considered at high risk if you were overweight or obese before pregnancy, have a family history of diabetes, or had gestational diabetes in a previous pregnancy.
Tests for gestational diabetes
Screening for gestational diabetes generally involves one or both of the following tests:
-
Initial glucose challenge test: You’ll drink a syrupy glucose solution, and your blood sugar will be measured after one hour.
-
A result of 190 mg/dL (10.6 mmol/L) or higher usually indicates gestational diabetes.
-
A reading below 140 mg/dL (7.8 mmol/L) is typically considered normal, but exact limits can vary by lab.
-
If your level is higher than normal, your doctor will recommend a follow-up test.
-
-
Follow-up glucose tolerance test: This test involves drinking a stronger glucose solution, with blood sugar measured every hour for three hours.
-
If two or more readings are higher than expected, the diagnosis of gestational diabetes is confirmed.
-
Treatment
Treatment for gestational diabetes focuses on keeping blood sugar levels within a healthy range to protect both you and your baby. The main components of treatment include lifestyle changes, blood sugar monitoring, and medication if needed.
Lifestyle changes
Making healthy lifestyle choices is essential to manage gestational diabetes. Because weight loss isn’t recommended during pregnancy, your doctor will help you set safe weight gain goals based on your pre-pregnancy weight.
Healthy habits include:
-
Eating a balanced diet: Focus on high-fiber, nutrient-rich foods that are low in fat and calories. Include fruits, vegetables, whole grains, and lean proteins. Limit refined carbohydrates such as white bread, rice, and sweets.
-
Working with a dietitian: A registered dietitian or certified diabetes educator can help create a personalized meal plan based on your nutritional needs, food preferences, and activity level.
-
Staying active: Regular physical activity lowers blood sugar and can ease pregnancy discomforts like back pain, swelling, and fatigue.
-
Aim for 30 minutes of moderate exercise most days, such as walking, swimming, or cycling.
-
Everyday movements like light housework or gardening also help.
-
Blood sugar monitoring
You’ll likely be asked to check your blood sugar several times a day, usually first thing in the morning and after meals. Regular testing helps ensure your levels stay in the target range.
Medicines
If lifestyle changes alone don’t control your blood sugar, your healthcare provider may prescribe insulin injections.
-
Insulin is considered safe during pregnancy and helps regulate blood sugar effectively.
-
Some providers may recommend oral medications, but their safety compared to insulin is still being studied.
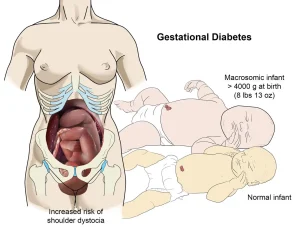
Monitoring your baby
Your healthcare team will closely monitor your baby’s growth and well-being with ultrasounds or other tests.
-
If you haven’t gone into labor by your due date, labor may be induced to prevent complications.
-
In some cases, induction may be recommended before your due date if your healthcare provider feels it’s safer for you and your baby.
Follow-up after delivery
Your blood sugar will be checked soon after birth and again within 6 to 12 weeks to ensure it has returned to normal.
-
If your blood sugar remains normal, you’ll still need testing every three years to monitor your risk of developing type 2 diabetes.
-
If you have prediabetes or type 2 diabetes after delivery, your healthcare team will create a long-term plan to manage it and maintain your health.
Advertisement