Overview
Diagnosis
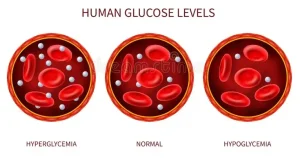
If you experience symptoms of low blood sugar, the first step is to check your blood sugar level using a blood glucose meter. This small device measures and displays your current blood sugar reading. For many people, hypoglycemia occurs when blood sugar drops below 70 mg/dL (3.9 mmol/L), though the exact number can vary. It’s important to discuss your target blood sugar range with your healthcare professional to understand what is normal for you.
Treatment
Treatment for diabetic hypoglycemia depends on the severity of your low blood sugar. If you suspect your blood sugar is low, check it immediately. If you can’t check it right away, assume it’s low and start treatment.
Managing hypoglycemia
Eat or drink carbohydrates
Consuming carbohydrates that are high in sugar helps raise your blood sugar quickly. Pure glucose is preferred and available in tablets, gels, and similar products. Foods with fat, like chocolate, work more slowly, and diet drinks are not effective because they contain no sugar.
Examples of foods that quickly raise blood sugar:
-
Glucose tablets or gels (follow the instructions on the package)
-
5–6 pieces of hard candy or jelly beans
-
4 ounces (½ cup) of fruit juice
-
4–6 ounces of regular (not diet) soda
-
1 tablespoon of sugar, honey, or corn syrup
Aim for 15–20 grams of carbohydrates to bring blood sugar back to a safe range.
Recheck your blood sugar
After 15 minutes, recheck your blood sugar. If it’s still low, take another 15–20 grams of carbohydrates. Repeat this cycle until your blood sugar is above 70 mg/dL (3.9 mmol/L).
Have a snack or meal
After recovery, eat a snack or meal to prevent another drop. If you use insulin, you may need to adjust your dose slightly when eating a full meal to avoid a sudden spike. Try not to overtreat low blood sugar, as this can cause high sugar levels and fatigue.
Children may need smaller carbohydrate doses, so ask a healthcare professional for guidance.
Emergency treatment
Severe hypoglycemia requires immediate treatment with glucagon, a hormone that raises blood sugar rapidly. Glucagon is available only by prescription and comes as:
-
An emergency syringe kit
-
An auto-injector pen or pre-mixed injection
-
A nasal spray powder
When giving glucagon to an unconscious person, turn them on their side to prevent choking if vomiting occurs. After about 15 minutes, they should become alert and able to eat. If not, seek emergency medical help.
If you use glucagon, inform your healthcare team afterward to determine whether your diabetes treatment plan needs adjustment.
Hard-to-manage hypoglycemia
If you frequently experience severe hypoglycemia despite medication changes, your healthcare professional may suggest keeping your blood sugar slightly higher. You might also use a continuous glucose monitor (CGM), which checks blood sugar every few minutes using a small sensor under the skin. Your provider may also advise carrying glucagon at all times and ensuring close contacts know how to use it.
Hypoglycemia unawareness
Some people don’t notice the early signs of low blood sugar — this is called hypoglycemia unawareness. If this happens, your healthcare provider may recommend keeping blood sugar targets higher and using a CGM that alerts you when your glucose drops. Checking your blood sugar before bed and having a small snack if levels are low can help prevent overnight hypoglycemia.
Self care
Teach people how to help
Inform trusted family, friends, and coworkers about your hypoglycemia. Teach them what symptoms to look for and how to use glucagon if needed.
Plan ahead
Always carry a source of fast-acting carbohydrates such as glucose tablets, hard candy, or regular soda. Keep glucagon with you if prescribed.
Wear a medical ID
Wear a medical ID bracelet or necklace that states you have diabetes. Carry a medical alert card in your wallet in case of emergencies.
Preparing for your appointment
If you experience frequent low blood sugar episodes, schedule a visit with your healthcare professional. Bring detailed information to help identify causes and solutions.
What you can do:
-
Ask if you need to fast before any blood tests
-
Record symptoms, frequency, and blood sugar readings
-
Note any recent stress or lifestyle changes
-
List all medications, vitamins, and supplements
-
Bring your glucose meter for review
-
Prepare questions such as:
-
How often should I check my blood sugar?
-
What is my target range?
-
How do diet, exercise, or weight changes affect my sugar?
-
How can I prevent both low and high blood sugar?
-
Should I have glucagon at home or work?
-
What to expect from your doctor
Your healthcare professional may ask questions such as:
-
What symptoms do you experience when blood sugar is low?
-
How often do these symptoms occur?
-
What do you do to raise your blood sugar?
-
What is your usual diet and exercise routine?
-
Do people around you know how to help during severe hypoglycemia?
Understanding your habits and patterns helps your healthcare team adjust your diabetes management plan and reduce the risk of future hypoglycemia episodes.
Advertisement