Overview
Diagnosis
The American College of Obstetricians and Gynecologists (ACOG) recommends that all pregnant individuals, regardless of age, be offered screening and diagnostic tests for Down syndrome.
-
Screening tests indicate the likelihood that the baby has Down syndrome but cannot confirm it.
-
Diagnostic tests can confirm whether the baby has Down syndrome.
Your healthcare provider will discuss the available tests, including their benefits, risks, and limitations, and may refer you to a genetic counselor for further guidance.
Screening Tests During Pregnancy
Screening for Down syndrome is a routine part of prenatal care. These tests estimate risk levels and help determine whether diagnostic testing is needed.
Common screening options include the first trimester combined test and the integrated screening test.
The First Trimester Combined Test
This test involves two steps:
-
Blood test: Measures PAPP-A (pregnancy-associated plasma protein-A) and HCG (human chorionic gonadotropin). Abnormal levels may indicate potential chromosomal issues.
-
Nuchal translucency ultrasound: Measures the fluid-filled space at the back of the baby’s neck. Extra fluid may signal chromosomal abnormalities such as Down syndrome.
The results, combined with the mother’s age, help estimate the risk of Down syndrome.
Integrated Screening Test
This test combines results from both the first and second trimesters for more accurate risk assessment.
-
First trimester: Blood test to measure PAPP-A and an ultrasound for nuchal translucency.
-
Second trimester: Quad screen that measures four pregnancy-related substances — alpha-fetoprotein, estriol, HCG, and inhibin A.
Cell-Free DNA Testing
A cell-free DNA (cfDNA) test analyzes small fragments of fetal DNA in the mother’s bloodstream to detect extra chromosome 21 material.
-
The test can be done from 10 weeks of pregnancy.
-
If the result is positive, a diagnostic test (CVS or amniocentesis) is needed to confirm the finding.
Diagnostic Tests During Pregnancy
If your screening test is positive or inconclusive, or if you have a high-risk pregnancy, diagnostic testing can provide a definitive answer.
Diagnostic options include:
-
Chorionic villus sampling (CVS):
-
Conducted between 10–14 weeks of pregnancy.
-
Involves collecting placental cells to study the baby’s chromosomes.
-
Carries a very low risk of miscarriage.
-
-
Amniocentesis:
-
Performed after 15 weeks of pregnancy.
-
Uses a needle to withdraw amniotic fluid for chromosomal analysis.
-
Also carries a very low miscarriage risk.
-
-
Preimplantation genetic testing (PGT):
-
Available for couples undergoing in vitro fertilization (IVF).
-
Embryos are tested for genetic abnormalities before implantation.
-
Diagnostic Tests for Newborns
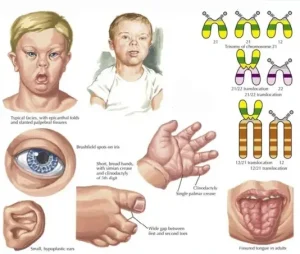
A physical examination is often enough to suspect Down syndrome in a newborn. To confirm, doctors perform a chromosomal karyotype test using a blood sample.
If an extra chromosome 21 (full or partial) is found in all or some cells, the diagnosis of Down syndrome is confirmed.
Treatment
Early intervention is essential for improving the quality of life in children with Down syndrome. Because every child is unique, treatment plans are personalized to meet individual developmental and medical needs.
Ongoing support — including healthcare, education, and life skills programs — helps children achieve their full potential.
Team Care
Managing Down syndrome typically involves a multidisciplinary care team to provide comprehensive support. This team may include:
-
Primary care pediatrician for general health coordination.
-
Cardiologist for heart-related issues.
-
Gastroenterologist for digestive health.
-
Endocrinologist for hormone and thyroid conditions.
-
Developmental pediatrician for growth and milestones.
-
Neurologist for nervous system concerns.
-
ENT specialist, ophthalmologist, and audiologist for sensory care.
-
Speech-language pathologist, physical therapist, and occupational therapist for developmental support.
Families should build a trusted network of medical professionals, educators, and therapists who can help access local and national support programs.
Some areas also offer Down syndrome specialty clinics, where multiple specialists collaborate in one location for integrated care.
Adults with Down Syndrome
As children with Down syndrome grow into adulthood, healthcare needs evolve. Regular medical checkups remain crucial, including monitoring for conditions that are more common in adults with Down syndrome.
Common health issues include:
-
Vision and hearing problems
-
Dental issues
-
Hypothyroidism
-
Diabetes
-
Celiac disease and GERD
-
Heart disease, stroke, and high cholesterol
-
Obesity
-
Sleep apnea
-
Mood and behavioral changes
-
Alzheimer’s disease
-
Arthritis, spine, and bone problems
Care should also address life planning needs, such as:
-
Living arrangements
-
Social and recreational opportunities
-
Employment and support programs
-
Financial assistance
-
Guardianship and legal planning
Advertisement