Overview
Diagnosis
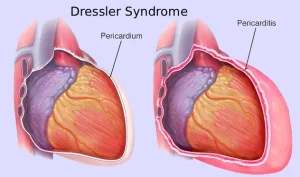
Diagnosis of Dressler syndrome begins with a physical examination by a healthcare professional. During the exam, the doctor listens to your heart using a stethoscope. A distinct sound called a pericardial rub may be heard if the pericardium is inflamed or fluid has collected around the heart.
Tests to Diagnose Dressler Syndrome
Several tests help confirm the presence of Dressler syndrome and assess inflammation or fluid buildup around the heart:
-
Complete Blood Count (CBC): Most people with Dressler syndrome have an elevated white blood cell count, indicating inflammation.
-
Inflammation Blood Tests:
-
C-reactive protein (CRP): A higher CRP level suggests inflammation caused by the immune response.
-
Erythrocyte Sedimentation Rate (ESR): A faster sedimentation rate means more inflammation.
-
-
Electrocardiogram (ECG or EKG):
-
Measures the heart’s electrical activity using electrodes attached to the chest, arms, and legs.
-
Detects signal changes suggesting pressure or inflammation around the heart.
-
However, ECG results may overlap with post-surgical changes, so additional tests are needed for confirmation.
-
-
Chest X-ray:
-
Detects fluid around the heart or lungs.
-
Helps differentiate Dressler syndrome from other conditions like pneumonia.
-
-
Echocardiogram:
-
Uses sound waves to create heart images.
-
Shows whether fluid is accumulating around the heart.
-
-
Cardiac MRI:
-
Provides detailed images of the heart’s structure and blood flow.
-
Can show pericardial thickening, confirming inflammation.
-
Treatment
The primary goals of Dressler syndrome treatment are to reduce inflammation and manage pain. Treatment often begins with medication, but surgery may be needed if complications arise.
Medications
The main treatment involves anti-inflammatory drugs (NSAIDs) to control inflammation and discomfort:
-
Aspirin — commonly used, especially after a heart attack.
-
Ibuprofen (Advil, Motrin IB, etc.) — helps reduce inflammation and pain.
-
Colchicine (Colcrys, Gloperba, etc.) — lowers inflammation and reduces recurrence risk.
-
Indomethacin — may also be prescribed in some cases.
If these medications fail to relieve symptoms, corticosteroids may be considered. These reduce inflammation by suppressing the immune system, but they:
-
Have serious side effects.
-
May delay heart tissue healing after a heart attack or surgery.
Thus, corticosteroids are used only when other treatments don’t work.
Surgery or Other Procedures
Surgical or interventional procedures may be required for complications of Dressler syndrome:
-
Draining Excess Fluid (Pericardiocentesis):
-
Used to treat cardiac tamponade, a life-threatening buildup of fluid around the heart.
-
A needle or catheter removes the fluid under local anesthesia.
-
-
Pericardiectomy:
-
Recommended for constrictive pericarditis, when the pericardium becomes stiff or scarred.
-
The surgery involves removing the pericardium to restore heart function.
-
Preparing for Your Appointment
If you visit the emergency room for chest pain, your healthcare professional may ask key questions to assess your condition, such as:
-
When did your symptoms begin?
-
How severe is your chest pain (on a scale of 1–10)?
-
Does anything worsen the pain, such as deep breathing or movement?
-
Where exactly is the pain located? Does it radiate beyond the chest?
-
Have you recently had a heart attack, heart surgery, or chest trauma?
-
Do you have a history of heart disease?
-
What medications are you currently taking?
Advertisement