Overview
Diagnosis
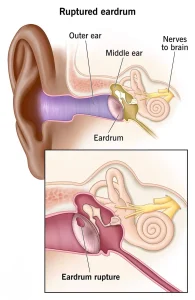
A ruptured eardrum is often diagnosed during an ear exam using an otoscope, a tool with a light that allows a healthcare professional or ENT specialist to see the eardrum clearly. Additional tests may be used to determine the cause of symptoms or check for hearing loss. Lab tests can analyze fluid draining from the ear to identify a bacterial infection. A tuning fork test may help detect hearing loss and determine whether the issue is related to the middle ear, inner ear or both. Tympanometry measures eardrum movement in response to changes in air pressure and can identify a tear. An audiology exam, done in a soundproof booth, evaluates hearing at different volumes and pitches.
Treatment
Most ruptured eardrums heal on their own within a few weeks. If an infection is present, antibiotic ear drops may be prescribed. When the tear does not heal naturally, procedures to close the hole may be recommended. An eardrum patch placed by an ENT specialist uses a chemical to stimulate healing and a small patch to cover the tear. This may need to be repeated more than once. If patching is not effective, surgery may be required. Tympanoplasty, the most common procedure, uses the person’s own tissue to close the hole and is typically done on an outpatient basis.
Self care
A ruptured eardrum often heals without intervention, but it is important to protect the ear while it recovers. Until cleared by a healthcare professional, keep the ear dry by using a waterproof silicone earplug or a cotton ball coated with petroleum jelly when bathing. Avoid cleaning the ears to prevent irritation. Do not blow the nose, as the pressure can disrupt healing.
Preparing for your appointment
If you have symptoms of a ruptured eardrum, you will likely start with a visit to your primary healthcare professional and may be referred to an ENT specialist. Before the appointment, prepare a list that includes your symptoms and when they began, any past ear infections or recent injuries, recent travel or exposure to loud noises, all medications you take and questions you want answered.
What to expect from your doctor
Your healthcare professional may ask questions about symptoms that have improved, past ear infections, exposure to loud sounds, recent swimming or diving, recent flights, head injuries or whether anything has been placed in the ear. These details help determine the cause of the perforation and guide treatment.
What you can do in the meantime
If you suspect a ruptured eardrum, keep the ear dry to avoid infection. Do not swim until your healthcare professional confirms it is safe. Use a waterproof earplug or a cotton ball coated with petroleum jelly while showering or bathing. Avoid using ear drops unless they are prescribed specifically for an infection related to the perforation.
Advertisement