Overview
Diagnosis
To diagnose end-stage renal disease (ESRD), healthcare providers perform a thorough assessment that includes medical history, physical examination, and specific diagnostic tests to evaluate kidney function and detect damage.
• Medical and family history:
Your provider reviews your family background, past illnesses, medications, and lifestyle factors that may contribute to kidney disease.
• Physical and neurological exams:
These help identify signs of fluid retention, nerve problems, or high blood pressure associated with kidney dysfunction.
• Blood tests:
Blood tests measure waste products like creatinine and urea, which build up when kidneys aren’t functioning properly.
• Urine tests:
Urine is analyzed for albumin (protein) and other substances to assess kidney filtration and damage.
• Imaging tests:
Tests such as ultrasound, MRI, or CT scans help evaluate kidney structure, size, and abnormalities.
• Kidney biopsy:
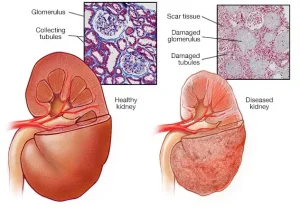
A small tissue sample is removed and examined under a microscope to determine the type and extent of kidney damage.
• Monitoring over time:
Some tests are repeated periodically to track the progression of kidney disease.
Stages of Kidney Disease
The stages of kidney disease are based on the glomerular filtration rate (GFR) — the amount of blood filtered by the kidneys each minute.
| Kidney Disease Stage | GFR (mL/min) | Kidney Function |
|---|---|---|
| Stage 1 | 90 or above | Healthy kidney function |
| Stage 2 | 60–89 | Mild loss of function |
| Stage 3a | 45–59 | Mild to moderate loss |
| Stage 3b | 30–44 | Moderate to severe loss |
| Stage 4 | 15–29 | Severe loss of function |
| Stage 5 | Less than 15 | Kidney failure (End-stage) |
End-stage renal disease (Stage 5) occurs when kidney function is below 15%, and the kidneys can no longer maintain essential bodily functions.
Treatment
Treatment for end-stage renal disease focuses on replacing lost kidney function or providing supportive care to manage symptoms and improve quality of life.
• Kidney transplant:
A surgical procedure where a healthy kidney from a living or deceased donor is placed into your body. This restores kidney function, eliminating the need for dialysis. Post-surgery, immunosuppressive medications prevent organ rejection, and close monitoring ensures successful recovery.
• Dialysis:
When transplantation isn’t immediately possible, dialysis takes over kidney functions like filtering blood and maintaining fluid balance.
-
Peritoneal dialysis: Uses the lining of your abdomen (peritoneum) and a special fluid to filter waste at home.
-
Hemodialysis: Filters blood using a machine, either at a medical center or at home.
• Palliative or supportive care:
If you choose not to undergo dialysis or transplant, palliative care focuses on symptom management, comfort, and end-of-life planning. It can also be combined with other treatments to enhance quality of life.
Without a transplant or dialysis, kidney failure progresses over time, leading to life-threatening complications. Early detection and treatment are essential to prolong survival and improve well-being.
Advertisement