Overview
Diagnosis
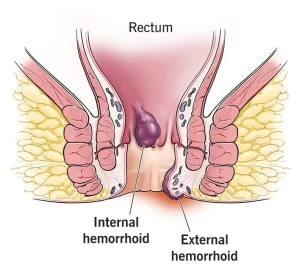
A healthcare professional can often identify external hemorrhoids through a simple visual examination. Diagnosing internal hemorrhoids, however, may require a more detailed evaluation of the anal canal and rectum.
The diagnostic process may include the following steps:
-
Digital exam: The healthcare professional inserts a gloved, lubricated finger into the rectum to check for abnormalities such as growths or swelling.
-
Visual exam: Since internal hemorrhoids are too soft to detect by touch, the doctor may use a special instrument like an anoscope, proctoscope, or sigmoidoscope to view the lower rectum and colon.
In some cases, a healthcare professional may recommend a colonoscopy to examine the entire colon, particularly if:
-
Symptoms suggest another digestive condition.
-
The patient has risk factors for colorectal cancer.
-
The patient is middle-aged and has not recently had a colonoscopy.
Specialized centers such as Mayo Clinic provide comprehensive evaluation and care for hemorrhoid-related health concerns, ensuring accurate diagnosis and individualized treatment.
Treatment
Treatment for hemorrhoids focuses on reducing symptoms such as pain, swelling, and inflammation. Mild cases can often be managed at home, while more severe or persistent hemorrhoids may require medical or surgical intervention.
Home remedies
Simple lifestyle changes and home treatments can help relieve discomfort and support healing:
-
Eat high-fiber foods such as fruits, vegetables, and whole grains to soften stool and prevent straining. Introduce fiber gradually to reduce gas.
-
Use topical treatments like over-the-counter creams, ointments, or suppositories containing hydrocortisone, witch hazel, or numbing agents.
-
Soak in a warm bath or sitz bath for 10 to 15 minutes several times a day to ease pain and swelling.
-
Take oral pain relievers such as acetaminophen, ibuprofen, or aspirin to manage temporary discomfort.
Symptoms usually improve within a week of home treatment. If pain or bleeding persists, it’s important to see a healthcare professional promptly.
Medicines
For mild cases, healthcare professionals may recommend over-the-counter products containing witch hazel, hydrocortisone, or lidocaine. These ingredients help relieve itching, swelling, and pain.
Hydrocortisone creams should not be used for more than a week without medical advice, as long-term use can thin the skin.
External hemorrhoid thrombectomy
If a blood clot develops within an external hemorrhoid, a healthcare professional can remove it through a minor procedure called a thrombectomy. This quick treatment, performed under local anesthesia, provides immediate relief and is most effective within 72 hours of clot formation.
Minimally invasive procedures
For hemorrhoids that cause persistent bleeding or severe pain, minimally invasive treatments can be performed in an outpatient setting without general anesthesia. These include:
-
Rubber band ligation: A small rubber band is placed around the base of an internal hemorrhoid to cut off its blood supply, causing it to shrink and fall off within a week.
-
Sclerotherapy: A chemical solution is injected into the hemorrhoid to shrink it. This method causes minimal pain but may be less effective than rubber band ligation.
-
Coagulation therapy: Techniques using laser, infrared light, or heat are used to harden and shrink small internal hemorrhoids. This approach typically causes little discomfort.
Surgical procedures
Surgery is usually reserved for severe or recurring hemorrhoids that don’t respond to other treatments. Common surgical options include:
-
Hemorrhoidectomy: Surgical removal of hemorrhoidal tissue. It is the most effective method for treating large or recurring hemorrhoids. Pain and temporary urinary difficulty can occur after the procedure, but medications and warm baths can help relieve symptoms.
-
Hemorrhoid stapling (stapled hemorrhoidopexy): This procedure blocks blood flow to the hemorrhoidal tissue and is generally used for internal hemorrhoids. Recovery is faster and less painful than hemorrhoidectomy, but there is a higher risk of recurrence and complications such as rectal prolapse or infection.
Discuss all available options with a healthcare professional to determine the most suitable treatment plan based on the severity of your symptoms and overall health.
Advertisement