Overview
Diagnosis
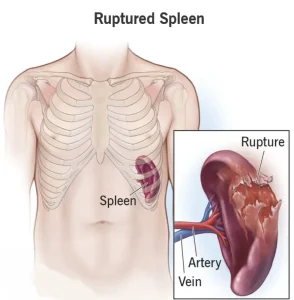
Diagnosing a ruptured spleen typically involves a combination of physical examination, lab tests and imaging. During a physical exam, a healthcare provider gently presses the abdomen to assess the spleen’s size and check for tenderness. Blood tests are often done to measure platelet count and evaluate how well the blood clots. In emergency situations, the medical team may check for internal bleeding with an ultrasound or by using a needle to draw fluid from the abdominal cavity. Finding blood in this fluid sample often leads to immediate surgical evaluation. If the diagnosis remains unclear, imaging tests such as a CT scan with or without contrast dye may be recommended to confirm the cause of symptoms.
Treatment
Treatment depends on the severity of the rupture. Severe cases typically require immediate surgery. Many mild to moderate spleen injuries can heal without an operation. In these situations, the patient is monitored in the hospital, and supportive care such as blood transfusions may be provided if needed. Follow-up CT scans may be used to track healing or to determine if surgery becomes necessary.
Surgery and other procedures
Surgical options vary based on the extent of the injury. In some cases, the spleen can be repaired using stitches or other techniques. When repair is not possible, removal of the spleen, or splenectomy, may be necessary. Although people can live without a spleen, losing it increases the risk of serious bacterial infections. Vaccinations against meningitis, pneumonia and Hib may be recommended, and some individuals may need daily antibiotics to reduce infection risk. In certain cases, only part of the spleen is removed. A partial splenectomy helps lower infection risks compared to removing the entire spleen. As with any surgery, risks include bleeding, infection, blood clots and pneumonia.
Advertisement