Overview
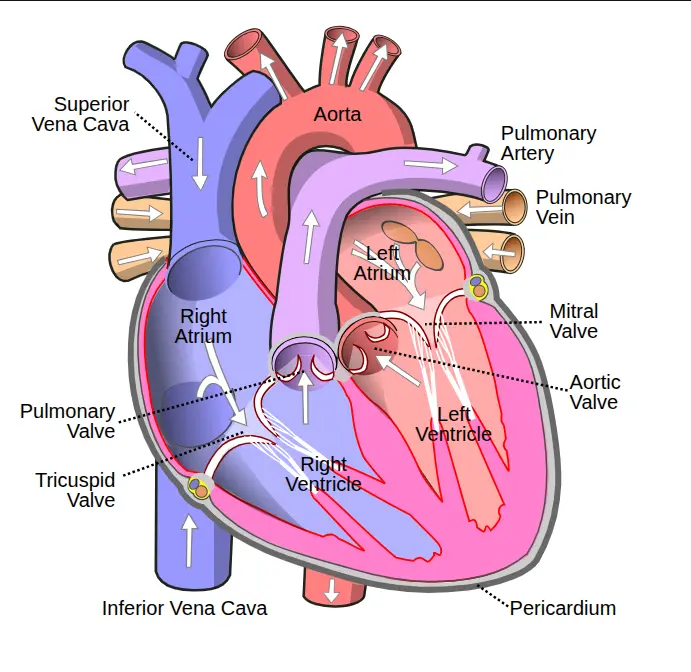
Aortic valve disease is a form of heart valve disease in which the valve between the lower left chamber of the heart, called the left ventricle, and the body’s main artery, called the aorta, does not function properly. The aortic valve plays a key role in keeping blood flowing in the correct direction from the heart to the rest of the body. When the valve is damaged or diseased, normal blood flow can be disrupted, placing extra strain on the heart.
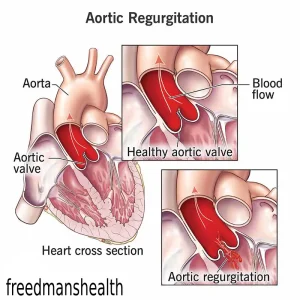
Aortic valve disease includes two main conditions. Aortic valve stenosis occurs when the valve flaps, also known as cusps, become thick, stiff, or fused together. This narrowing limits blood flow out of the heart. Aortic valve regurgitation occurs when the valve does not close completely, allowing blood to leak backward into the left ventricle.
Some people are born with aortic valve disease as part of a congenital heart defect, while others develop it later in life due to age-related changes or other medical conditions. Treatment depends on the type and severity of disease and may include monitoring, medications, or surgery to repair or replace the valve.
Symptoms
Some individuals with aortic valve disease may have no symptoms for many years. When symptoms occur, they may include:
-
Chest pain or a feeling of tightness
-
Dizziness or lightheadedness
-
Fainting
-
Fatigue, especially after physical activity
-
Reduced ability to exercise or be active
-
Irregular or pounding heartbeat
-
Shortness of breath, particularly during exertion or when lying down
In children with aortic valve stenosis, symptoms may include poor appetite and failure to gain weight as expected.
Causes
Aortic valve disease can be caused by a heart condition present at birth, known as a congenital heart defect. In other cases, the disease develops later in life due to various factors, including:
-
Age-related wear and tear of the valve
-
Infections affecting the heart
-
Long-standing high blood pressure
-
Injury to the heart
The heart contains four valves that ensure one-way blood flow: the aortic, mitral, tricuspid, and pulmonary valves. Each valve has flaps that open and close with every heartbeat. In aortic valve disease, these flaps may become thick and stiff or may fail to close properly, impairing blood flow from the left ventricle into the aorta.
Risk factors
Several factors increase the risk of developing aortic valve disease:
-
Older age, as calcium buildup can stiffen the aortic valve over time
-
Congenital heart defects involving abnormal valve structure
-
History of rheumatic fever following untreated strep throat
-
Endocarditis, an infection of the heart’s inner lining and valves
-
Prior radiation therapy to the chest
-
Certain health conditions, such as chronic kidney disease, lupus, or Marfan syndrome
These factors can contribute to valve narrowing, leakage, or both.
Complications
If left untreated, aortic valve disease can lead to serious complications, including:
-
Formation of blood clots
-
Stroke
-
Heart failure
-
Abnormal heart rhythms, known as arrhythmias
-
Sudden cardiac arrest and death
Early diagnosis and appropriate treatment can significantly reduce the risk of these complications and improve long-term outcomes.
Prevention
Not all cases of aortic valve disease can be prevented, especially those related to congenital defects or aging. However, certain steps may help lower risk or slow progression:
-
Treat strep throat promptly to prevent rheumatic fever
-
Manage blood pressure and other heart-related conditions
-
Practice good dental hygiene to reduce the risk of endocarditis
-
Attend regular medical checkups if you have known heart valve abnormalities
-
Follow recommended care if you have conditions that increase valve disease risk
Ongoing monitoring and early intervention are essential for maintaining heart health in people at risk of aortic valve disease.
Advertisement