Overview
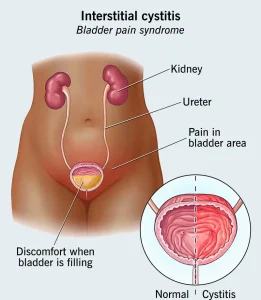
Interstitial cystitis, also known as painful bladder syndrome, is a chronic condition characterized by bladder pressure, bladder pain, and discomfort in the pelvic region. Unlike urinary tract infections, interstitial cystitis is not caused by bacteria and does not respond to antibiotics. The severity of symptoms can vary over time, with periods of flare-ups and remission.
Symptoms
-
Chronic pelvic pain or bladder pain
-
Persistent urge to urinate
-
Frequent urination, often in small amounts
-
Pain or discomfort that worsens as the bladder fills and improves after urination
-
Pain during sexual intercourse
-
Discomfort in the lower abdomen or urethra
Causes
The exact cause of interstitial cystitis is unknown. Possible contributing factors include:
-
Defects in the bladder lining that allow irritating substances in urine to penetrate
-
Autoimmune reactions
-
Nerve dysfunction increasing pain sensitivity
-
Previous bladder infections or trauma
-
Genetic predisposition
Risk factors
-
Female gender
-
Middle age
-
History of chronic pain conditions such as irritable bowel syndrome or fibromyalgia
-
Family history of interstitial cystitis
Complications
-
Reduced bladder capacity due to chronic inflammation
-
Persistent pelvic pain affecting daily activities
-
Sleep disturbances due to frequent urination
-
Sexual dysfunction
-
Emotional distress, anxiety, or depression
Prevention
There is no known way to prevent interstitial cystitis, but symptom management strategies may help reduce flare-ups:
-
Identifying and avoiding trigger foods or beverages
-
Bladder training techniques to increase time between urination
-
Stress management practices
-
Pelvic floor physical therapy when recommended
-
Following treatment plans prescribed by healthcare providers
Although interstitial cystitis has no cure, a combination of lifestyle changes, therapies, and medications can help manage symptoms and improve quality of life.
Advertisement