Overview
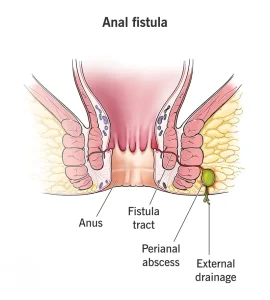
An anal fistula, also known as fistula-in-ano, is an abnormal tunnel that forms between the inside of the anus and the skin surrounding the anus. The anus is the muscular opening at the end of the digestive tract through which stool exits the body.
Most anal fistulas develop as a result of an infection in an anal gland. This infection can lead to an abscess, which may drain on its own or be surgically drained through the skin near the anus. After drainage, a tunnel may remain open, connecting the infected anal gland or anal canal to an opening on the outer skin.
In most cases, surgery is required to treat an anal fistula. Depending on the type and complexity of the fistula, nonsurgical treatments may occasionally be considered.
Symptoms
Symptoms of an anal fistula can vary depending on the severity and location of the tunnel. Common symptoms include:
-
An opening on the skin near the anus
-
Redness, swelling or irritation around the external opening
-
Discharge of pus, blood or stool from the opening
-
Pain or discomfort in the anus or rectum, especially when sitting or during bowel movements
-
Fever or a general feeling of illness
Symptoms may come and go, especially if the fistula drains intermittently.
Causes
Anal fistulas most commonly result from an infection that begins in an anal gland. When the gland becomes infected, it can form an abscess. Once the abscess drains, either naturally or through surgery, a tunnel may remain under the skin.
This tunnel connects the infected anal gland or anal canal to an opening in the skin around the anus, forming a fistula. The presence and path of the fistula are influenced by the anal sphincter muscles, which control bowel movements.
Fistulas are classified based on how they pass through or around the sphincter muscles. This classification is important, as it helps guide treatment decisions and reduces the risk of complications.
Risk factors
Certain conditions and situations can increase the risk of developing an anal fistula.
Common risk factors include:
-
A previously drained anal abscess
-
Crohn’s disease or other inflammatory bowel diseases
-
Trauma or injury to the anal area
-
Infections affecting the anal region
-
Surgery or radiation therapy for anal cancer
Anal fistulas occur most frequently in adults around the age of 40. They may also develop in younger individuals, particularly those with Crohn’s disease. Anal fistulas are more common in males than in females.
Complications
Even with appropriate treatment, anal fistulas can recur. Recurrent abscess formation may lead to repeated infections and additional fistula development.
Surgical treatment carries certain risks, including potential damage to the anal sphincter muscles. In some cases, this can result in difficulty controlling bowel movements, a condition known as fecal incontinence. The risk depends on the fistula’s location and the type of treatment used.
Prevention
There is no guaranteed way to prevent an anal fistula, but reducing the risk of anal infections may help. Prompt treatment of anal abscesses and infections can lower the chance of fistula formation.
Managing underlying conditions such as Crohn’s disease, maintaining good anal hygiene and seeking medical care for persistent anal pain, swelling or discharge may help reduce complications and support early intervention.
Advertisement