Overview
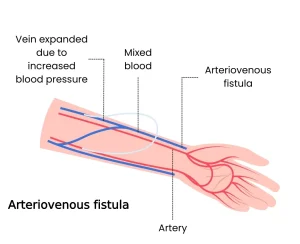
An arteriovenous (AV) fistula is an abnormal connection between an artery and a vein. Under normal conditions, blood flows from arteries into smaller blood vessels called capillaries, and then into veins. The capillaries allow oxygen and nutrients in the blood to be delivered to body tissues.
In an arteriovenous fistula, blood flows directly from an artery into a vein, bypassing the capillaries. When this occurs, tissues that normally receive blood through those capillaries may get less oxygen and fewer nutrients.
Arteriovenous fistulas most commonly develop in the legs but can occur anywhere in the body. In some people with advanced kidney disease, an AV fistula is intentionally created through surgery to allow easier access for dialysis.
Symptoms of an arteriovenous fistula depend on its size and location. Small fistulas may cause no problems and only require monitoring. Larger or untreated fistulas can lead to serious complications. Treatment options may include observation, compression, catheter-based procedures or surgery.
Symptoms
Small arteriovenous fistulas in the arms, legs, lungs, kidneys or brain often cause no noticeable symptoms. These fistulas are frequently discovered during imaging tests performed for other reasons and may not require treatment beyond regular monitoring.
Larger arteriovenous fistulas may cause symptoms such as:
-
Purplish, bulging veins visible under the skin, similar to varicose veins
-
Swelling in the arms or legs
-
Low blood pressure
-
Fatigue
-
Heart failure
A significant arteriovenous fistula in the lungs, known as a pulmonary arteriovenous fistula, is a serious condition and may cause:
-
Pale gray or bluish lips or fingernails due to reduced oxygen levels
-
Rounding and widening of the fingertips, known as clubbing
-
Coughing up blood
An arteriovenous fistula in the digestive tract may lead to bleeding in the gastrointestinal tract.
When to see a doctor
If you notice symptoms that may suggest an arteriovenous fistula, schedule an appointment with a health care provider. Early diagnosis can make treatment more effective and may reduce the risk of complications such as blood clots or heart failure.
Causes
Arteriovenous fistulas may be present at birth or may develop later in life.
Possible causes include:
-
Injuries that pierce the skin, such as gunshot or stab wounds, especially when an artery and vein are close together
-
Congenital arteriovenous fistulas, which occur when arteries and veins do not develop normally before birth
-
Genetic conditions that affect blood vessel formation, such as hereditary hemorrhagic telangiectasia, also called Osler-Weber-Rendu disease
-
Dialysis-related surgery, in which an arteriovenous fistula is surgically created to support long-term dialysis in people with end-stage kidney disease
Risk factors
Certain conditions and factors may increase the risk of developing an arteriovenous fistula.
These include:
-
Congenital or genetic blood vessel disorders
-
Older age
-
Female sex
-
Cardiac catheterization procedures, particularly those involving blood vessels in the groin
-
Use of certain medications, including blood thinners and medications that affect bleeding
-
High blood pressure
-
Increased body mass index
Complications
If left untreated, an arteriovenous fistula can lead to serious complications.
One of the most serious complications is heart failure. Large arteriovenous fistulas allow blood to flow rapidly from arteries to veins, forcing the heart to work harder. Over time, this strain can weaken the heart and lead to heart failure.
Blood clots may form, particularly in fistulas located in the legs. These clots can cause deep vein thrombosis, which can be life-threatening if a clot travels to the lungs and causes a pulmonary embolism. Depending on the location, clots may also increase the risk of stroke.
Reduced blood flow to muscles may cause leg pain during activity, a condition known as claudication.
Internal bleeding may occur if an arteriovenous fistula affects organs such as the stomach or intestines.
Prevention
Not all arteriovenous fistulas can be prevented, especially those present at birth. However, certain steps may reduce the risk of acquired fistulas and related complications.
Preventive measures include:
-
Managing high blood pressure
-
Maintaining a healthy body weight
-
Following medical advice after procedures involving blood vessels
-
Monitoring known congenital or genetic conditions that affect blood vessels
-
Seeking prompt medical care for penetrating injuries
Regular medical checkups and early evaluation of unusual symptoms can help detect arteriovenous fistulas before serious complications develop.
Advertisement