Overview
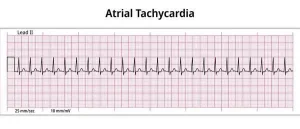
Atrial tachycardia is a type of irregular heartbeat, also called an arrhythmia. It belongs to a group of heart rhythm disorders known as supraventricular tachycardias, which originate in the upper chambers of the heart, called the atria.
During an episode of atrial tachycardia, the heart beats faster than normal, often exceeding 100 beats per minute. In many cases, the heart rate rises to 150 to 200 beats per minute before returning to a normal resting rate of about 60 to 80 beats per minute. Episodes may begin gradually or start suddenly and can stop just as quickly.
Atrial tachycardia is relatively common and may occur in people who are otherwise healthy. It is more frequently seen in individuals who have had heart surgery or during pregnancy. Certain triggers, such as infections, stimulant medications or alcohol use, can bring on episodes.
Symptoms
The most common symptom of atrial tachycardia is a rapid heartbeat that feels much faster than normal. The fast heart rate may occur suddenly or last for an extended period.
Other symptoms may include:
-
Pounding, fluttering or racing sensations in the chest or neck, known as palpitations
-
Chest pain or discomfort
-
Lightheadedness or dizziness
-
Fainting or feeling close to fainting
-
Shortness of breath
-
Sweating
-
Weakness or extreme fatigue
-
Nausea
Some people with atrial tachycardia may not notice any symptoms, especially if episodes are brief or infrequent.
Symptoms can be harder to recognize in infants and young children. In these age groups, atrial tachycardia may cause poor feeding, excessive sweating, irritability or changes in skin color. A healthcare professional should be consulted if these signs are present.
Causes
Atrial tachycardia is caused by abnormal electrical signals in the heart. Normally, electrical impulses travel through the heart in an organized pattern that controls the heart rate and rhythm.
In atrial tachycardia, faulty electrical signals begin too early in the atria. This abnormal activity causes the heart to beat faster than normal. When the heart beats too quickly, it may not have enough time to fill with blood between beats, which can reduce how effectively blood is pumped throughout the body.
Risk factors
Atrial tachycardia can occur in anyone, but certain conditions and lifestyle factors increase the risk.
Medical risk factors include:
-
Coronary artery disease and other heart diseases
-
Heart valve disease
-
Heart failure
-
Congenital heart defects present at birth
-
Previous heart surgery
-
Sleep apnea
-
Thyroid disorders
-
Lung diseases, including chronic obstructive pulmonary disease
-
Diabetes
Other factors that may increase the risk include:
-
Emotional stress
-
Excessive caffeine intake
-
Heavy alcohol use
-
Smoking or nicotine use
-
Use of stimulant drugs such as cocaine or methamphetamine
-
Certain medications, including some used to treat asthma, allergies and colds
Complications
Atrial tachycardia is usually not life-threatening, especially in people without underlying heart disease. However, frequent or prolonged episodes can become a concern.
Possible complications include weakening of the heart muscle if the rapid heartbeat continues for long periods. In people with existing heart conditions or heart damage, atrial tachycardia may worsen symptoms and increase the risk of other heart rhythm problems. Early evaluation and appropriate management can help reduce the risk of complications.
Advertisement