Overview
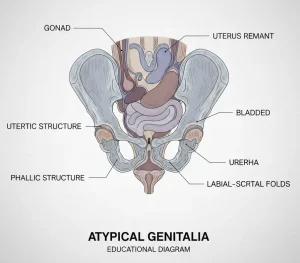
Atypical genitalia, previously known as ambiguous genitalia, is a rare condition in which a newborn’s external sex organs do not appear clearly male or female. In some infants, the genitals may be underdeveloped, appear different from typical male or female anatomy, or show features of more than one sex. The appearance of the external genitals may not match the internal sex organs or the genetic sex, which is usually determined by sex chromosomes, most often XX or XY.
External genitals include structures such as the clitoris, labia, penis, scrotum and the vaginal opening. Internal genitals include organs such as the uterus, ovaries, fallopian tubes, prostate and testicles. The ovaries and testicles, also called gonads, produce sex hormones that guide sexual development. Genetic sex is established at conception and is typically XX for females and XY for males.
Atypical genitalia is not a disease but a variation in sex development. It is usually identified at birth or shortly afterward. The diagnosis can be emotionally challenging for families. Healthcare teams focus on identifying the cause, providing clear information and offering counseling to help guide decisions about sex assignment and any necessary medical care.
Symptoms
Atypical genitalia is most often noticed by healthcare professionals soon after birth, though it may sometimes be suspected before delivery. The physical appearance varies widely and depends on the timing and nature of hormonal or genetic influences during fetal development.
In infants with XX chromosomes, possible features include:
-
An enlarged clitoris that may resemble a penis
-
Labia that are fused or appear similar to a scrotum
-
Lumps within the fused labia that may feel like testicles
In infants with XY chromosomes, possible features include:
-
An opening of the urethra on the underside of the penis, known as hypospadias
-
A very small penis with the urethral opening closer to the scrotum
-
One or both testicles not present in the scrotum
-
Undescended testicles with an empty scrotum that may resemble labia, with or without a very small penis
Causes
Atypical genitalia usually result from disruptions in hormone production or hormone response during pregnancy, which interfere with normal development of the sex organs. These changes occur while the fetus is developing in the womb.
Genetic sex is determined at conception, when an egg carrying an X chromosome is fertilized by a sperm carrying either an X or a Y chromosome. All fetuses initially develop from the same basic tissue. Whether this tissue becomes male or female sex organs depends on chromosomes and the presence or absence of hormones called androgens, which promote male genital development.
In fetuses with a Y chromosome, specific genetic signals lead to the formation of testicles, which produce androgens. These hormones drive the development of male genitalia. In the absence of a Y chromosome and without androgen effects, female genital development occurs.
Atypical genitalia can develop when these steps are altered. Reduced androgen production or action in a genetic male fetus can result in incomplete male genital development. Exposure to excess androgens in a genetic female fetus can cause masculinization of the external genitals. Genetic mutations, chromosomal variations and certain syndromes affecting multiple organ systems may also be involved. In some cases, the exact cause cannot be identified.
Possible causes in genetic females include:
-
Congenital adrenal hyperplasia, which leads to excess androgen production
-
Exposure before birth to medications or conditions that increase androgen levels
-
Rare hormone-producing tumors in the pregnant individual
Possible causes in genetic males include:
-
Abnormal testicle development
-
Androgen insensitivity syndrome, in which tissues do not respond properly to androgens
-
Disorders affecting testosterone production or action
-
5-alpha-reductase deficiency, which interferes with the conversion of testosterone into its active form
Risk Factors
Family history plays an important role, as many differences of sex development are linked to inherited genetic changes. Factors that may increase risk include a family history of:
-
Unexplained deaths in early infancy
-
Infertility, absent menstrual periods or excessive facial hair in females
-
Atypical genitalia
-
Unusual physical development during puberty
-
Congenital adrenal hyperplasia
Families with these histories may benefit from genetic counseling before pregnancy.
Complications
Potential complications depend on the underlying cause and individual anatomy. Possible complications include:
-
Infertility, which varies based on the specific condition
-
Increased risk of certain cancers associated with some differences of sex development
With appropriate medical care, counseling and long-term follow-up, many individuals with atypical genitalia can lead healthy lives.
Prevention
There is no known way to prevent atypical genitalia, as many causes are genetic or occur early in fetal development. Genetic counseling may help families with a known history of differences of sex development understand potential risks and plan future pregnancies. Early diagnosis and coordinated care can help reduce complications and support long-term health and well-being.
Advertisement