Overview
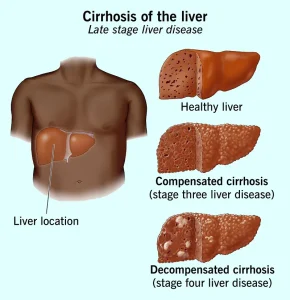
Cirrhosis is a chronic liver condition in which healthy liver tissue is gradually replaced by scar tissue, leading to permanent damage and impaired liver function. This scarring disrupts normal blood flow through the liver and interferes with essential processes such as detoxification, protein production, digestion, and nutrient metabolism.
Cirrhosis develops over many years as a result of ongoing liver injury. In its early stages, the liver may still function adequately, but as scarring progresses, liver failure and serious complications can occur.
Symptoms
Symptoms of cirrhosis often do not appear until significant liver damage has occurred. As the disease advances, symptoms become more noticeable.
Common symptoms include:
-
Fatigue and weakness
-
Loss of appetite
-
Nausea
-
Unexplained weight loss
-
Swelling of the legs, ankles, or abdomen
-
Yellowing of the skin and eyes
-
Itchy skin
-
Easy bruising or bleeding
-
Dark urine and pale stools
-
Confusion, difficulty concentrating, or memory problems
Symptoms vary depending on the severity of liver damage.
Causes
Cirrhosis is caused by long-term liver injury that leads to inflammation and scarring.
Common causes include:
-
Chronic alcohol misuse
-
Chronic viral hepatitis, especially hepatitis B and C
-
Nonalcoholic fatty liver disease
-
Autoimmune hepatitis
-
Bile duct diseases
-
Genetic liver disorders
-
Long-term exposure to toxins or certain medications
Multiple causes may contribute to liver damage in some individuals.
Risk Factors
Several factors increase the risk of developing cirrhosis.
These include:
-
Heavy or long-term alcohol consumption
-
Chronic hepatitis infection
-
Obesity and metabolic syndrome
-
Diabetes
-
Family history of liver disease
-
Long-term use of medications that affect the liver
-
Exposure to environmental toxins
Managing these risk factors can reduce disease progression.
Complications
As cirrhosis progresses, it can lead to life-threatening complications due to impaired liver function and increased pressure in the portal vein.
Possible complications include:
-
Portal hypertension
-
Ascites
-
Variceal bleeding
-
Hepatic encephalopathy
-
Increased risk of liver cancer
-
Kidney dysfunction
-
Infections due to weakened immunity
Advanced cirrhosis often requires specialized medical care.
Prevention
While not all cases of cirrhosis can be prevented, many can be avoided by reducing liver injury and managing underlying conditions.
Preventive measures include:
-
Limiting or avoiding alcohol consumption
-
Getting vaccinated against hepatitis A and B
-
Practicing safe behaviors to reduce hepatitis transmission
-
Maintaining a healthy weight
-
Managing diabetes and cholesterol levels
-
Avoiding unnecessary or harmful medications
-
Undergoing regular liver health checkups when at risk
Early detection and consistent management are key to slowing progression and improving long-term outcomes for individuals with cirrhosis.
Advertisement