Overview
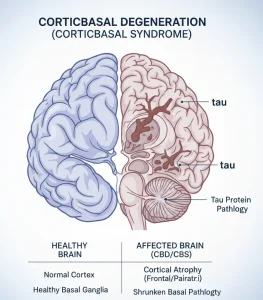
Corticobasal degeneration, also known as corticobasal syndrome, is a rare, progressive neurodegenerative disorder that affects movement, thinking, and behavior. It is characterized by gradual damage to specific areas of the brain, particularly the cerebral cortex and basal ganglia. The condition usually begins in adulthood and worsens over time, leading to increasing physical and cognitive impairment.
Symptoms
Symptoms of corticobasal degeneration vary between individuals and often affect one side of the body more than the other, especially in early stages. Common symptoms include:
-
Progressive stiffness or rigidity of one limb
-
Difficulty with coordinated movements, such as using the hands
-
Muscle jerking or involuntary movements
-
Tremors or abnormal postures
-
Problems with speech, including slurred or slow speech
-
Difficulty swallowing
-
Cognitive impairment, including problems with memory, planning, or judgment
-
Changes in behavior or personality
-
Apraxia, or difficulty performing learned movements despite normal strength
Causes
The exact cause of corticobasal degeneration is unknown. It is associated with the abnormal accumulation of a protein called tau in brain cells, which leads to cell damage and loss of normal brain function. These protein changes disrupt communication between brain regions involved in movement and cognition. The condition is generally sporadic and not inherited in most cases.
Risk Factors
Factors that may increase the risk of corticobasal degeneration include:
-
Increasing age, most commonly affecting individuals over 50
-
No clear genetic inheritance pattern in most cases
-
Possible association with certain neurodegenerative processes
-
Unknown environmental or biological factors
Complications
As corticobasal degeneration progresses, it can lead to significant complications:
-
Severe mobility limitations and loss of independence
-
Frequent falls and injury
-
Speech and swallowing difficulties leading to aspiration
-
Progressive cognitive decline and dementia
-
Muscle contractures and chronic pain
-
Increased need for long-term care and support
Prevention
There is currently no known way to prevent corticobasal degeneration. However, supportive care can help manage symptoms and improve quality of life:
-
Early evaluation by a neurologist for persistent movement or cognitive symptoms
-
Physical, occupational, and speech therapy to maintain function
-
Use of assistive devices to improve safety and mobility
-
Regular monitoring for swallowing and nutritional issues
-
Support for caregivers and long-term care planning
Advertisement