Overview
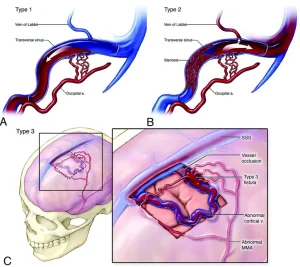
Dural arteriovenous fistulas are abnormal connections between arteries and veins that occur within the dura mater, the outer protective covering of the brain and spinal cord. These abnormal connections disrupt normal blood flow, causing high-pressure arterial blood to flow directly into veins. The condition can range from mild and asymptomatic to severe and life-threatening, depending on the location and blood flow pattern.
Symptoms
Symptoms vary widely based on the fistula’s size, location, and drainage pattern:
-
Persistent or pulsating headaches
-
Ringing or whooshing sound in the ears
-
Visual disturbances
-
Dizziness or balance problems
-
Seizures
-
Weakness or numbness in limbs
-
Cognitive or behavioral changes
-
Stroke-like symptoms in severe cases
-
Sudden neurological deterioration if bleeding occurs
Causes
Dural arteriovenous fistulas may develop due to several underlying factors:
-
Abnormal blood vessel formation in the dura mater
-
Head or spinal trauma
-
Prior brain or spinal surgery
-
Blood clots in dural venous sinuses
-
Infections affecting the central nervous system
-
Spontaneous development without a clear cause
Risk Factors
Certain conditions increase the likelihood of developing dural arteriovenous fistulas:
-
History of head injury
-
Previous neurosurgical procedures
-
Venous sinus thrombosis
-
Advanced age
-
Male sex
-
Chronic infections or inflammation
-
Connective tissue abnormalities
Complications
If left untreated, dural arteriovenous fistulas can lead to serious complications:
-
Intracranial hemorrhage
-
Ischemic or hemorrhagic stroke
-
Progressive neurological deficits
-
Increased intracranial pressure
-
Vision loss
-
Seizures
-
Cognitive decline
-
Life-threatening brain injury
Prevention
There is no guaranteed method to prevent dural arteriovenous fistulas, but risk reduction strategies may help:
-
Prompt treatment of head injuries
-
Early management of venous blood clots
-
Regular medical follow-up after brain or spinal surgery
-
Managing infections effectively
-
Seeking medical evaluation for unexplained neurological symptoms
Advertisement