Overview
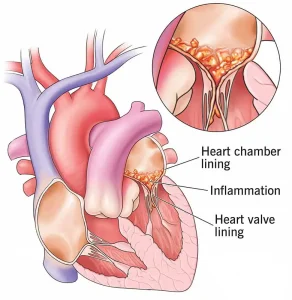
Endocarditis is a serious and potentially life-threatening infection of the inner lining of the heart chambers and heart valves, known as the endocardium. It occurs when bacteria, fungi, or other microorganisms enter the bloodstream and attach to damaged areas of the heart. Endocarditis can damage heart valves and disrupt normal blood flow, requiring prompt diagnosis and treatment.
Symptoms
Symptoms of endocarditis may develop slowly or appear suddenly, depending on the cause and severity. Common symptoms include:
-
Fever and chills
-
Fatigue and weakness
-
Shortness of breath
-
Heart murmur or change in an existing heart murmur
-
Night sweats
-
Muscle and joint aches
-
Persistent cough
-
Swelling of the feet, legs, or abdomen
-
Unexplained weight loss
Causes
Endocarditis is caused by microorganisms that enter the bloodstream and settle on the heart lining or valves. This may occur due to:
-
Bacteria from the mouth, skin, or intestines entering the blood
-
Invasive medical or dental procedures
-
Intravenous drug use
-
Indwelling medical devices such as catheters
-
Existing heart valve damage or congenital heart defects
Risk Factors
Several factors increase the risk of developing endocarditis, including:
-
Artificial or damaged heart valves
-
Previous history of endocarditis
-
Congenital heart disease
-
Poor dental hygiene or gum disease
-
Intravenous drug use
-
Long-term use of intravenous lines
Complications
If not treated promptly, endocarditis can cause severe complications, such as:
-
Heart valve destruction and heart failure
-
Stroke or other embolic events
-
Abscess formation in the heart or other organs
-
Persistent or spreading infection
-
Kidney damage
-
Life-threatening heart rhythm disturbances
Prevention
Preventing endocarditis involves reducing the risk of bloodstream infections, especially in high-risk individuals. Preventive measures include:
-
Maintaining good oral hygiene and regular dental care
-
Prompt treatment of infections
-
Using antibiotics before certain dental or medical procedures when recommended
-
Avoiding intravenous drug use
-
Proper care and monitoring of medical devices
Early diagnosis and appropriate treatment are essential to prevent serious complications and improve outcomes in individuals with endocarditis.
Advertisement