Overview
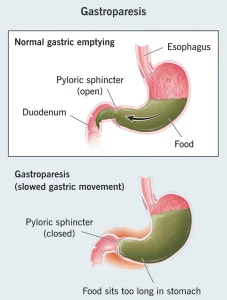
Gastroparesis is a digestive disorder in which the stomach empties food into the small intestine more slowly than normal. This delay occurs without a physical blockage and is usually related to problems with the nerves or muscles that control stomach movement. Gastroparesis can interfere with digestion, blood sugar control, and proper nutrition, and symptoms may range from mild to severe.
Symptoms
Symptoms of gastroparesis often develop gradually and may worsen after meals. Common symptoms include:
-
Nausea
-
Vomiting of undigested food
-
Feeling full after eating small amounts
-
Abdominal bloating
-
Upper abdominal pain
-
Loss of appetite
-
Unintentional weight loss
-
Acid reflux
-
Fluctuating blood sugar levels, especially in people with diabetes
Symptoms may vary depending on how severely stomach emptying is delayed.
Causes
Gastroparesis occurs when the nerves or muscles of the stomach do not function properly. Common causes include:
-
Diabetes-related nerve damage
-
Injury to the vagus nerve during surgery
-
Neurological disorders such as Parkinson’s disease or multiple sclerosis
-
Viral infections affecting stomach nerves
-
Use of certain medications that slow digestion
-
Unknown causes, referred to as idiopathic gastroparesis
In many cases, no clear cause can be identified.
Risk Factors
Several factors increase the risk of developing gastroparesis, including:
-
Long-standing diabetes
-
Previous stomach or esophageal surgery
-
Neurological or autoimmune disorders
-
Use of opioid pain medications or certain antidepressants
-
Female sex
These factors can disrupt normal stomach muscle contractions.
Complications
Gastroparesis can lead to several complications if not managed properly. Possible complications include:
-
Poor nutrition due to reduced food intake
-
Dehydration from frequent vomiting
-
Formation of hardened food masses called bezoars
-
Unstable blood sugar levels
-
Reduced quality of life due to chronic symptoms
Long-term complications may require ongoing medical care.
Prevention
Gastroparesis cannot always be prevented, especially when related to nerve damage or chronic illness. However, certain measures may help reduce risk or severity:
-
Maintaining good blood sugar control in diabetes
-
Eating smaller, more frequent meals
-
Avoiding high-fat and high-fiber foods that slow digestion
-
Staying hydrated
-
Following medical advice after stomach or nerve-related surgery
Early diagnosis and proper dietary and medical management can help control symptoms and prevent complications.
Advertisement