Overview
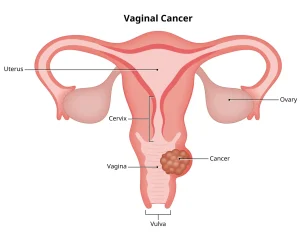
Vaginal cancer is a rare type of cancer that begins in the tissues of the vagina, the muscular tube connecting the uterus to the external genitalia. It most commonly affects older adults, particularly after menopause, but it can occur at any age. The most frequent type is squamous cell carcinoma, which develops from the thin, flat cells lining the vaginal surface.
Vaginal cancer often develops slowly and may begin as precancerous changes known as vaginal intraepithelial neoplasia (VAIN). Early-stage vaginal cancer may not cause noticeable symptoms, making regular gynecological examinations important for early detection.
Symptoms
Symptoms of vaginal cancer may be mild or absent in the early stages and become more noticeable as the disease progresses. Common symptoms include:
-
Abnormal vaginal bleeding, especially after menopause or after intercourse
-
Watery, bloody, or foul-smelling vaginal discharge
-
Pain during sexual intercourse
-
Pelvic pain or discomfort
-
A lump or mass in the vagina
-
Painful urination or frequent urge to urinate
-
Constipation in advanced cases
Causes
Vaginal cancer occurs when normal vaginal cells develop genetic changes that cause uncontrolled growth. While the exact cause is not always clear, several factors are known to increase the risk of these cellular changes.
Key causes and contributing factors include:
-
Long-term infection with high-risk human papillomavirus (HPV)
-
Progression from untreated vaginal intraepithelial neoplasia
-
Prior cervical cancer or cervical precancer
-
Previous radiation therapy to the pelvic area
Risk Factors
Several factors can increase the risk of developing vaginal cancer:
-
Age over 60 years
-
Persistent HPV infection
-
Smoking
-
History of cervical cancer or abnormal Pap test results
-
Weakened immune system
-
Exposure to diethylstilbestrol (DES) before birth
Complications
Vaginal cancer and its treatment can lead to various physical and emotional complications:
-
Pain and difficulty during sexual activity
-
Urinary or bowel problems
-
Vaginal narrowing or scarring after radiation therapy
-
Infertility in younger individuals
-
Emotional distress, anxiety, or depression
Prevention
Although vaginal cancer cannot always be prevented, certain measures can significantly reduce risk and support early detection:
-
Regular gynecological checkups and Pap tests as recommended
-
HPV vaccination to protect against high-risk HPV strains
-
Avoiding smoking
-
Practicing safe sex to reduce HPV transmission
-
Early treatment and monitoring of precancerous vaginal changes
Early diagnosis and timely treatment improve outcomes and help maintain quality of life.
Advertisement