Overview
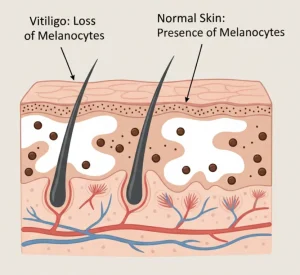
Vitiligo is a long-term skin condition in which patches of skin lose their normal pigmentation, resulting in white or light-colored areas. This occurs when the immune system mistakenly attacks the melanocytes, the cells responsible for producing skin pigment (melanin).
Vitiligo can affect any part of the body, including the face, hands, arms, and genitals. The condition is not contagious, but it can impact emotional well-being and self-esteem due to its visible nature. The exact cause is not fully understood, but autoimmune factors, genetics, and environmental triggers are thought to play a role.
Symptoms
The main symptom of vitiligo is the appearance of depigmented patches on the skin. Other symptoms may include:
-
White or lighter-colored patches on the skin, often symmetrical
-
Premature graying of hair on the scalp, eyebrows, eyelashes, or beard
-
Loss of color in the mucous membranes (mouth and nose)
-
Loss of color in the retina of the eye in some cases
-
Patches that gradually enlarge over time
Vitiligo often progresses slowly, but the rate and pattern vary widely among individuals.
Causes
Vitiligo occurs when melanocytes are destroyed or stop functioning, leading to a loss of skin pigment. Factors that contribute include:
-
Autoimmune response targeting melanocytes
-
Genetic predisposition, as it sometimes runs in families
-
Environmental triggers such as skin trauma, sunburn, or stress
-
Neurochemical factors that may damage melanocytes
The condition is not caused by infection or poor hygiene.
Risk Factors
Certain factors increase the likelihood of developing vitiligo:
-
Family history of vitiligo or other autoimmune diseases
-
Presence of other autoimmune conditions, such as thyroid disease, type 1 diabetes, or rheumatoid arthritis
-
Exposure to significant skin trauma or sunburn
-
Stressful life events
-
Age under 30, as vitiligo often appears early in life
Complications
Vitiligo is primarily a cosmetic condition, but it can lead to physical and emotional challenges:
-
Increased sensitivity to sunlight in affected areas
-
Eye problems in rare cases
-
Hearing loss if melanocytes in the inner ear are affected
-
Emotional and psychological impact, including low self-esteem, anxiety, or depression
-
Social or occupational challenges due to visible skin changes
Prevention
There is no known way to prevent vitiligo, but early intervention may help manage progression:
-
Avoiding skin trauma and sunburn
-
Using sunscreen to protect depigmented areas
-
Seeking early treatment from a dermatologist to slow spread
-
Managing stress and underlying autoimmune conditions
-
Regular monitoring for other autoimmune disorders
Although vitiligo cannot be fully cured, treatments such as topical medications, light therapy, and cosmetic camouflage can help improve appearance and quality of life.
Advertisement