Overview
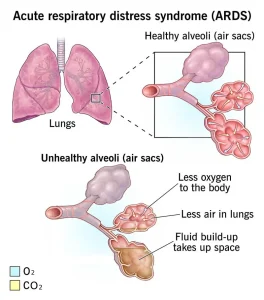
Acute respiratory distress syndrome (ARDS) is a serious condition that occurs when swelling in the lungs causes fluid to leak into the tiny air sacs, known as alveoli. These air sacs normally allow oxygen to pass into the bloodstream. When fluid builds up, the lungs cannot fill with enough air, and oxygen levels in the blood drop.
As a result, vital organs such as the brain, heart and kidneys do not receive enough oxygen to function properly. ARDS most often develops in people who are already critically ill or who have experienced severe injury. Symptoms usually appear within hours to a few days after the triggering illness or injury.
ARDS is life-threatening. The risk of death increases with age and the severity of the underlying condition. Some people recover fully, but others are left with long-term lung damage and ongoing health problems.
Symptoms
The severity of ARDS symptoms varies depending on the cause and whether there is existing heart or lung disease.
Common symptoms include:
-
Severe shortness of breath
-
Rapid and labored breathing that is not normal for the person
-
Cough
-
Chest discomfort or tightness
-
Fast heart rate
-
Confusion
-
Extreme tiredness or weakness
When to see a doctor
ARDS usually develops in people who are already hospitalized due to serious illness or injury. If symptoms of ARDS occur outside a medical facility, emergency medical care is needed immediately.
Severe breathing difficulty, confusion or sudden worsening of symptoms requires urgent evaluation at the nearest emergency department.
Causes
ARDS develops when fluid leaks into the alveoli due to damage or inflammation in the lungs. Several conditions can trigger this response.
Common causes include:
-
Sepsis, a severe and widespread bloodstream infection
-
Severe pneumonia affecting multiple areas of the lungs
-
Coronavirus disease 2019 (COVID-19), particularly severe cases
-
Major injuries to the head, chest or other parts of the body
-
Breathing in harmful substances such as smoke, chemical fumes, vomit or water during near-drowning
-
Other conditions such as acute pancreatitis, massive blood transfusions or severe burns
Risk factors
Most people who develop ARDS are already hospitalized and critically ill. Certain factors increase the risk.
Risk factors include:
-
Serious infections such as sepsis or pneumonia
-
Severe COVID-19 infection, especially with metabolic syndrome
-
Alcohol use disorder
-
Recreational drug use
-
Smoking or long-term tobacco use
-
A history of alcohol, drug or tobacco exposure
These factors can weaken lung defenses and increase vulnerability to lung injury.
Complications
ARDS can lead to serious complications during hospitalization and after recovery.
Possible complications include:
-
Blood clots, especially in the legs, which can travel to the lungs and cause a pulmonary embolism
-
Collapsed lung, known as pneumothorax, often related to ventilator pressure
-
Lung infections due to prolonged ventilator use
-
Permanent scarring and stiffening of lung tissue, called pulmonary fibrosis
-
Stress ulcers caused by increased stomach acid during critical illness
Even with improved survival rates, many ARDS survivors experience long-term effects.
Long-term complications may include:
-
Ongoing breathing problems and reduced lung capacity
-
Persistent shortness of breath and fatigue
-
Depression
-
Memory loss and difficulty thinking clearly
-
Muscle weakness and prolonged tiredness after hospitalization
Prevention
There is no guaranteed way to prevent ARDS, but reducing risk factors can help lower the chance of developing it.
Preventive measures include:
-
Prompt treatment of serious infections
-
Avoiding smoking and recreational drug use
-
Limiting alcohol intake
-
Using protective equipment when exposed to smoke or harmful chemicals
-
Seeking early medical care for severe illness or injury
Early recognition and intensive medical care are critical to improving outcomes in people with ARDS.
Advertisement